Jaundice and hepatitis
- 1. JAUNDICE & HEPATITIS PRESENTER- Ms. Anshu M.Sc Nursing KGMU Institute of Nursing
- 2. INTRODUCTION The term jaundice is derived from the French word “jaune” which means yellow. Jaundice is not a disease, but rather a visible sign of an underlying disease process.
- 3. Jaundice in adults can be caused by a variety of medical conditions, some of which are serious and potentially life- threatening. Any adult who develops jaundice needs to undergo a comprehensive medical evaluation in order to determine its cause.
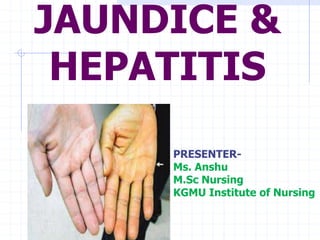
- 4. DEFINITION Jaundice is a yellowish discoloration of the skin, mucous membranes and of the white of the eyes caused by elevated levels of the chemical bilirubin in the blood (hyperbilirubinemia).
- 5. EPIDEMIOLOGY Jaundice typically present as a symptom of a disease. About 5% of the U.S population is thought to have jaundice due to hereditary causes. About 10% American population has jaundice due to cholelithiasis.
- 6. ANATOMY OF LIVER The liver is a large, highly vascular organ located behind the ribs in the upper right portion of the abdominal cavity. Weight=1200-1500g
- 8. PHYSIOLOGY OF LIVER • Cleans the blood • Regulates hormones • Helps with blood clotting • Produces bile • Produces important enzymes • Maintains blood sugar levels
- 9. Haemoglobin Metabolism Bilirubin is a product of metabolism of haemoglobin (80%) and other haem containing proteins (e.g. Myoglobin, cytochrome P450: 20%) Degredation of haemoglobin into bilirubin takes place in macrophages. Bilirubin is then excreted into plasma and binds with albumin
- 10. What is bilirubin? The breakdown product of Hgb from injured RBCs and other heme containing proteins. Produced by reticuloendothelial system (macrophage system) Released to plasma bound to albumin Hepatocytes conjugate it and extrete through bile channels into small intest.
- 11. BILE METABOLISM
- 12. What causes bilirubin? Overproduction by reticuloendothelial system Failure of hepatocyte uptake Failure to conjugate or excrete Obstruction of biliary excretion into intestine
- 15. Pathophysiology
- 17. TYPES OF JAUNDICE Hemolytic jaundice Hepatocellular jaundice Obstructive jaundice Hereditary hyperbilirubinemia
- 18. HEMOLYTIC JAUNDICE Hemolytic jaundice is the result of an increased destruction of the RBC, the effect of which is to flood the plasma with bilirubin so rapidly. But the liver is functioning normally.
- 19. HEPATOCELLULAR JAUNDICE Caused by the inability of damaged liver cells to clear normal amount of bilirubin from the blood. Causes- Hepatitis Medications or chemical toxins(carbon tetrachloride, chloroform, phosphorus) alcohol
- 20. OBSTRUCTIVE JAUNDICE Results from extrahepatic obstruction may be caused by occlusion of bile duct from a gallstone, an inflammatory process, a tumor or pressure from an enlarge organ
- 22. HEREDITARY HYPERBILIRUBINEMIA Increased serumbilirubin levels resulting from any of several inherited diorders, can also produce jaundice. Eg- Gilbert’s syndrome- increased level of unconjugated bilirubin that causes jaundice.
- 23. RISK FACTORS Heavy alcohol consumption Pancreatitis Liver cirrhosis Viral hepatitis
- 24. SIGNS AND SYMPTOMS pale-colored stools, dark-colored urine, skin itching, nausea and vomiting, Yellow sclera diarrhea,
- 25. fever and chills, weakness, weight loss, loss of appetite, confusion, abdominal pain, headache Yellowish skin
- 26. Clinical Features Painless jaundice in older person with epigastric mass & weight loss = biliary obstruction from malignancy Hepatomegaly with pedal edema, JVD, and gallop = CHF
- 27. COMPLICATIONS Chronic hepatitis Cancer Liver failure Kidney failure Hepatic encephalopathy (brain dysfunction) Death
- 28. Laboratory Tests Hitory of patient Physical examination Serum bilirubin level (total and direct)- 0.3-1gm/dl Liver aminotransferase levels- sGPT- Alk. Phos - U/A for bilirubin and urobilogen
- 29. CBC PT Coombs test Hgb electrophoresis Viral hepatitis panel U/S Gallbladder
- 30. abdominal ultrasound computerized tomography (CT)scan magnetic resonance imaging (MRI) cholescintigraphy (HIDA scan).
- 31. PREVENTION OF JAUNDICE Avoid high-risk behaviors such as - unprotected intercourse • intravenous drug use implement universal precautions when working with blood products and needles. This can decrease your risk of developing hepatitis B or hepatitis C.
- 32. vaccination against hepatitis A and hepatitis B. There is currently no available vaccine against hepatitis C. Avoid potentially contaminated food products or unsanitary water, as this may decrease your risk of developing hepatitis A.
- 33. When travelling to areas where malaria is endemic, take the recommended precautions and prophylactic medications in order to prevent the development of malaria. Avoid alcohol and smoking, as it is a risk factor for the development of pancreatic cancer, as well as many other malignancies.
- 34. MANAGEMENT GOAL- To relief symptoms To prevent complications
- 35. 1. Pain management- give analgesics 2. Antibiotics 3. IV fluids – to prevent dehydration 4. Blood Transfusion- in case of anaemia and haemolysis 5. Anti-viral therapy
- 36. Neonatal Jaundice 1. Physiological jaundice 2. Pathological jaundice
- 37. NURSING MANAGEMENT ASSESSMENT- Assess for general condition of patient. Assess for pain Assess for any other complication
- 38. NURSING DIAGNOSIS Acute pain related to disease condition Imbalanced Nutrition Less Than Body Requirements related to nausea and vomiting Impaired skin integrity related to pruritis
- 39. HEALTH EDUCATION AND DISCHARGE TEACHING Encourage for healthy diet. Advice for consumption of clean food and water. Hand hygiene Safe intercourse Adhere to medication
- 41. HEPATITIS DEFINITION- Hepatitis refers to an inflammatory condition of the liver
- 42. Etiology Can have many causes Drugs (Bromfenac,Troglitazone,Pemoline etc) toxins alcohol viral infections (A, B, C, D, E) other infections (parasites, bacteria) physical damage
- 43. PATHOPHYSIOLOGY Due to etiology Exposure to hepatitis virus Infection and inflammation of liver Hepatocyte damage Necrosis of the parts of liver, alteration of liver function
- 44. Hepatitis Terms Acute Hepatitis: Short-term hepatitis. Body’s immune system clears the virus from the body within 6 months Chronic Hepatitis: Long-term hepatitis. Infection lasts longer than 6 months because the body’s immune system cannot clear the virus from the body
- 45. Types Hepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E
- 46. Hepatitis A What is it? Infection of the liver caused by Hepatitis A virus Incubation period 30 days on average (range 15-50 days)
- 47. Geographic Distribution of HAV Infection HAV Prevalence High Intermediate Low very Low
- 48. Hepatitis A TRANSMITION - by consuming food or water contaminated by feces from a person infected with hepatitis A.
- 49. Hepatitis A Prevention Shot of immunoglobulin up to 2 weeks after exposure Good hand washing Cook food well Good diaper hygiene Only drink clean water VACCINation- Children after 12 months Adults 18 yrs or old (combo of hep A and hep B, given in 3 shots-0,1,6 months)
- 50. Hepatitis B What is it? Hep B is a serious disease caused by a Hep B virus that infects the liver Can cause lifelong infection, cirrhosis (liver scarring), liver cancer, liver failure and death
- 51. Geographic Distribution of Chronic HBV Infection HBsAg Prevalence 8% - High 2-7% - Intermediate <2% - Low
- 52. Hepatitis B Incubation period 1-6 months chronic carriers remain infectious
- 53. MODE OF TRANSMITION Transmitted through puncture wounds or contact with infectious body fluids, such as blood, saliva, or semen. Injection drug use having sex with an infected partner sharing razors of infected person
- 54. 10% 90% Chronically infected Clear the infection HEPATITIS B
- 55. Hepatitis B VACINATION- All babies- at birth, 1month (4weeks), 6month (24weeks)
- 56. Hepatitis C What is it? Hep C is a liver infection caused by a virus Also known as non A, non B hepatitis
- 57. Hepatitis C Incubation period 15-160 days chronic carriers remain infectious
- 58. Hepatitis C Shared injection equipment Blood transfusion Blood transfer ( tattoo, piercing) Sex Mother to child (<5%) • How it is transmitted ?
- 59. 85% 15% Chronically infected Clear the infection HEPATITIS C
- 60. Hepatitis C PREVENTION- Do not share injection equipment(it’s a universal precaution). Do not donate blood or plasma, organs or sperm Do not share toothbrushes, razors Cover areas of open skin Use of safer sex techniques
- 61. Hepatitis D This is also called delta hepatitis. Hepatitis D is a serious liver disease caused by the hepatitis D virus (HDV).
- 62. MODE OF TRANSMITION Transmitted through puncture wounds or contact with infected blood. Hepatitis D is a rare form of hepatitis that occurs in conjunction with hepatitis B infection
- 63. Hepatitis E Hepatitis E is a waterborne disease caused by the hepatitis E virus (HEV). Hepatitis E is mainly found in areas with poor sanitation and is typically caused by ingesting contaminated food and water.
- 64. COMMON SIGNS AND SYMPTOMS fatigue flu-like symptoms dark urine pale stool abdominal pain loss of appetite unexplained weight loss yellow skin and eyes, which may be signs of jaundice
- 65. Signs and Symptoms of Hepatitis There are three phases of Hepatitis – Preicteric Icteric Posticteric.
- 66. Preicteric phase nausea / vomiting decreased appetite / weight loss Fever Fatigue headache and joint pain rt upper quadrant abdominal pain enlarged spleen/liver/lymph nodes rash and itching of the skin (urticaria).
- 67. Icteric phase These symptoms include the symptoms of preicteric phase jaundice (yellowing of the skin) pruritus (intense / persistent itch) clay or light-colored stools and dark urine
- 68. Posticteric phase which involves the cessation of the above noted symptoms liver enlargement continued fatigue
- 69. Complications of Hepatitis chronic liver disease cirrhosis (scarring of the liver) cancer of the liver
- 70. DIAGNOSTICS TEST Complete history of patient Physical examination Serum bilirubin Liver function test Ultrasound Liver biopsy Viral Antibody Testing
- 71. MANAGEMENT GOAL- To minimize infectivity and liver inflammation To treat symptomatic causes To prevent complication
- 72. HEPATITIS A Hepatitis A isn’t usually treated. Bed rest may be recommended if symptoms cause a great deal of discomfort. For vomiting or diarrhoea give high fluid and caloric diet to prevent malnutrition or dehydration.
- 73. HEPATITIS B Acute hepatitis B doesn’t require specific treatment. Chronic hepatitis B is treated with antiviral medications. ANTIVIRAL THERAPY- Lamivudine adefovir
- 74. Hepatitis C Antiviral medications are used to treat both acute and chronic forms of hepatitis C Treatment Interferon A and Ribavirin (suggest 40% “cure” rate)
- 75. Hepatitis D Hepatitis D is treated with a medication called alpha interferon.
- 76. Hepatitis E There are currently no specific medical therapies to treat hepatitis E It typically resolves on its own. People with this type of infection are often advised to get adequate rest, drink plenty of fluids, get enough nutrients, and avoid alcohol.
- 77. NURSING MANAGEMENT ASSESSMENT- Assess for pain Assess for nausea, vomiting and diarrhoea Check and record for weight
- 78. Nursing Diagnosis: 1. Acute Pain related to swelling of the liver 2. Breathing Pattern related to intra- abdominal fluid collections ascites decreased lung expansion and accumulation of secretions 3. Imbalanced Nutrition Less Than Body Requirements related to nausea and vomiting
- 79. NURSING INTERVENTION 1. Acute pain related to swelling of the liver Monitor and record vital signs. assess the severity,frequency, and characteristic of pain. Provide divertional activities such as reading newspapers. administer medication as ordered.
- 80. 2.Imbalanced Nutrition Less Than Body Requirements related to nausea and vomiting Monitor the inclusion of diet / calories. Give a little meal in the frequency often. Provide oral care before meals. Encourage intake of orange juice, beverage and candy carbonate heavy throughout the day. Keep an eye on blood glucose.
- 81. 3.Impaired skin integrity related to pruritis Assess for pruritis. Nails of the patient should be cut short to prevent skin injury. Apply emollient, don’t leave the skin dry. Apply antibiotic ointment if any injury is present
- 82. HEALTH EDUCATION AND DISCHARGE TEACHING Get regular medical care Get needed rest No alcohol, no over the counter drug use Avoid chemical fumes and other environmental toxins Get vaccinated.
- 84. CONCLUSION HEPATITIS A B C D E Mode of transmission Faeco - oral Body fluid Body fluid Body fluid Faeco - oral Immunization available available Not available Not available Not available Severity More sever
- 85. CONCLUTION Liver is chemical factory of human body. Hepatitis is a viral infection which causes inflammation of liver. Its timely management is important to prevent complications.
- 86. EVALUATION
- 87. Questions 1) Unconjugated hyperbilirubinemia usually results from a intra- or extrahepatic biliary obstruction. A. True B. False Ans- (b)
- 88. 2) All patients with jaundice should be admitted to the hospital for further workup. A. True B. False Ans- (b)
- 89. 3) A marker of acute hepatocyte injury &/or hepatocyte death is: A. PT B. ALT C. Albumin D. Direct bilirubin E. Ammonia Ans- (b)
- 90. 4) In which of the following phase clay coloured stool is present? A) pre-icterus phase B) icterus phase C) post-icterus phase D) all phase Ans- b)