History taking format for gyne
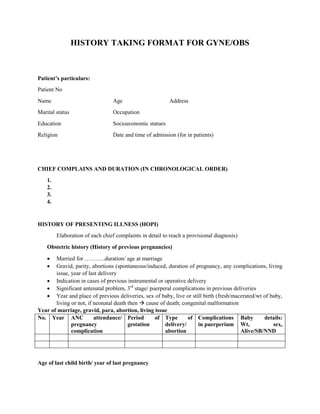
- 1. HISTORY TAKING FORMAT FOR GYNE/OBS Patient’s particulars: Patient No Name Age Address Marital status Occupation Education Socioeconomic statues Religion Date and time of admission (for in patients) CHIEF COMPLAINS AND DURATION (IN CHRONOLOGICAL ORDER) 1. 2. 3. 4. HISTORY OF PRESENTING ILLNESS (HOPI) Elaboration of each chief complaints in detail to reach a provisional diagnosis) Obstetric history (History of previous pregnancies) Married for ………..duration/ age at marriage Gravid, parity, abortions (spontaneous/induced, duration of pregnancy, any complications, living issue, year of last delivery Indication in cases of previous instrumental or operative delivery Significant antenatal problem, 3rd stage/ puerperal complications in previous deliveries Year and place of previous deliveries, sex of baby, live or still birth (fresh/macerated/wt of baby, living or not, if neonatal death then cause of death; congenital malformation Year of marriage, gravid, para, abortion, living issue No. Year ANC attendance/ pregnancy complication Period of gestation Type of delivery/ abortion Complications in puerperium Baby details: Wt, sex, Alive/SB/NND Age of last child birth/ year of last pregnancy
- 2. MENSTRUAL HISTORY: Age of menarche (k): …….years Duration of flow …..days/ length of cycle (from first day of one cycle to 1st day of next cycle) …..days ± ……days Regular/ irregular (range of shortes longest cycle) Amount of flow, any passage of clots, no of soaked pads/day fully soaked or not) Dysmenorrheal? Severity/duration Intermenstrual bleeding Post coital bleeding Last menstrual perid (LMP): 1st day of last normal menstrual period If menopausal ask about duration/age of menopause and post menopausal bleeding CONTRACEPTIVE HISTORY Type of contraception, duration, cause of discontinuation (if discontinued), date of discontinuation, date of last dose if using depo provera Duration between last child and current pregnancy PAST HISTORY Any medical or surgical history (Hx of TB, DM, HTN, epilepsy, endocrinal disorders, blood transfusion, cardiac disease/ any surgical interventions in the past) History of STDs, recurrent PID FAMILY HISTORY: Only primary relatives TB/DM/HTN/ female genital tract malignancies In Antenatal cases: multiple pregnancies, congenital anomalies (sp. Downs syndrome) PERSONAL HISTORY Smoking (duration and no of cigarettes per day); alcohol intake; allergy, etc TREATMENT HISTORY Any treatment done for present illness or any medication which the patient is taking regularly
- 3. SPECIAL POINTS TO CONSIDER IN HISTORY TAKING OF COMMON OBS/GYNE PROBLEMS: For antenatal cases: Duration of cessation of menses in months, LMP, EDD Gestation age in weeks Fetal movements; date of perception and whether normal or not (>10 /day) ANC attendance ( place/regularity and starting) TT immunization (no of doses, week at injection) Taking iron/calcium or folic acid Deworming done or not Any problems in each trimester e.g. severe vomiting, pain abdomen, fever, urinary problems, vaginal bleeding or abnormal discharge, severe headache, swelling/ any conditions requiring hospital admission during this pregnancy should be noted For labor cases (to be added in above history) Labor pain (duration in hours, continuous/intermittent, site, radiation, frequency, interval between pains (in minutes), duration of pain( in seconds), severity {true vs false} Blood stained mucoid discharge PV (show), amount, duration Leaking (watery discharge PV) duration, color and smell For postnatal cases (peurperium) Chief complain Day of delivery Type of delivery: normal (completed 37 weeks, singleton, vertex presentation, spontaneous vaginal delivery (ventouse/forcep) or cesarean section with indication. Other type of abnormal delivery should be specified e.g. preterm, twin pregnancy, breech vaginal delivery, etc Pain lower abdomen after delivery (after pains) Blood stained discharge P/V (lochia): color, amount, smell Pain at wound (perineal/abdominal) site, swelling, discharge, etc HOPI: She was admitted on ………….. at ……. With complaints of cessation of menses …… duration and pain abdomen………. Hrs. Any intervention during labor e.g. augmentation (iv oxytocin drip), artificial rupture of membrane,etc type, time outcome of delivery. Any third stage complications like post partum hemorrhage, retained palcenta. Lactation started or not, any breast problem lie crack nipple, engorgement or pain in breast. Urine passed/not after delivery, any bowel problems. Fever, pain in legs. Any other problems after delivery. Condition of the baby ANC Visit detail, any antenatal complications
- 4. FOR PAIN LOWER ABDOMEN: Duration, mode of onset, site, severity, radiation, referred pain, character aggravating/relieving factor, relation to urinary/bowel symptoms, abnormal vaginal discharge, relation to menstrual cycle, any history of amernorrhea, dyspareunia FOR UTEROVAGINAL PROLAPSE Duration of something coming out per vagina, how it started, increasing or not, aggravated by straining/ coughing, etc , reducible spontaneously on lying downs, has to be reduced manually or not reducible Urinary problems’ leaking of urine on cough/laugh (stress incontinence), difficulty in passing urine, inability to hold urine (urge incontinence), increased frequency or burning micturition, retention, incomplete voiding, etc Bowel problems ( chronic constipation) History of chronic cough, smoking Smelly/blood stained discharge per vagina Previous treatment esp ring pessary of any surgical intervention for uv prolapsed In obstetric history: ask about prolonged/difficult labor, spacing between pregnancies, early resumption of heavy work in peurperium + other risk factors for UVP MASS IN ABDOMEN Duration, site of mass, onset Increasing or decreasing or same in size Pain, fever, discharge PV Association with menstrual problems: menorrhagia, metorrhagia, dysmennorhea Pressure symptoms: Urrinary retention; frequency; bowel problems, any change in bowel habit, swelling of lower limbs, etc Loss of wt, appetite VAGINAL DISCHARGE Durataion, type of discharge Occupation of both, possible multiple partners, contraceptive use Amount, color, smell, itching, pain lower abdomen, relation to menstrual cycle History of antibiotics intake, immunosupressants, OCPs Past history of vaginitis or cervicitis or PID Past and family history of DM INABILITY TO CONCEIVE (SUBFERTILITY) Age and occupation of both partners
- 5. Duration of marriage, duration/regularity of staying together Use of contraception Frequency of intercourse, awareness about fertility period, any problem in intercourse Any breast problems: galactorrhea Regularity of menstrual cycle Features suggestive of ovulation, regular cycle, premenstrual mastalgia, dysmenorrheal Any previous pregnancies: outcome, complications Any investigations or treatment done so far Past history of TB, recurrent PID, diabetes, thyroid disorder, pelvic surgeries Family history of TB, diabetes Drugs which may increase prolactin.. e.g phenothiazine, methyldopa, metoclopromide Smoking, alcohol abuse, drug abuse MENSTRUAL PROBLEMS OR ABNORMAL PV BLEEDING: Duration, type of proble in terms of amount, duration of cycle, length, regularity (recent 6-12 months cycle pattern) Passage of clots, fleshy mass, any preceeding amenorrhea Associated pain/mass in lower abdomen Drug use esp hormones. Anticoagulants Contraceptive use; eg OCPs, depo provera, norplant, IUCD History of thyroid disorder, history suggestive of bleeding disorder, prolonged bleeding from cut injuries, petechial rashes, bruises, gum bleeding etc Features associated with anemia: fatigue, palpitation, SOB, swelling, etc FORMAT FOR PHYSICAL EXAMINATION General examination: General condition: ill looking/fair, satisfactory, comfortable/distressed, built – average/thin/obese, hydration Height, weight (must in ANC) Cardinal signs: Pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema, dehydration {PICCLED} Vitals: Pulse; BP; respiratory rate; temperatyre Thyroid; breasts (symmetry, nipple, lump, tenderness) Cardiovascular system: Respiratory system
- 6. Abdomen: Inspection: ( contour, scars, pigmentation, linea niagra, stria gravidarum, stria albicans, venous prominences, umbilicus, hernial orifices, movement with respiration, any visible mass) Palpation: tenderness, organomegaly, abnormal mass, raised temperature, guarding, rigidity, In case of lump in abdomen: size, site, mobility, margin, surface, tenderness, lower border of mass reached or not Percussion: (fluid/gas/mass/organs) Auscultation: Bowel sounds Obstetrics (Antenatal Examination) (Supine position with slightly flexed thighs and knees) Fundal height in realtion to gestation weeks ( symphysis fundal measurement with tape is alternative method) —in cm ( after 20 weeks corresponds to WOG) Abdominal girth (in inches)—around the point of maximum buldge) Fundal grip ( 1st leopolds) Lateral grip ( 2nd leopolds) First and second pelvic grip ( 3rd and 4th ) ( These examinations will tell the student about fundal height, fetal lie, attitude, position, presentation and engagement of presenting part) Auscultation of fetal heart sound: rate/regularity Labor cases (in addition to above) Uterine contractions (duration, frequency, intensity) should be noted Postnatal cases: Height of uterus ( involution, weeks or cm) Uterus will be contracted or not, any tenderness In case of LSCS, site of wound, any soakage over dressing, bowel sounds Pelvic examination: In dorsal position, thighs and knees fully flexed and legs abducted ( patients should be examined with empty bladder, only condition to examine patient while full bladder is when checking for urinary stress incontinence) Inspection of external geitalia (pubic hair distribution, any laxity of introitus, any lesion, vaginal discharge, bleeding, descent of vaginal wall or cervix Per speculum examination (inspection of cervix, lateral vaginal wall, any lesion, bleeding, discharge or grwth Bimanual examination of uterus (size, position, whether anterverted or retroverted, mobility and tenderness, any abnormal mass/tenderness in lateral/anterior/posterior fornices), cervical motion tenderness
- 7. In labor cases Pain abdomen: duration, site, nature intensity, frequency, progressive Blood stained discharge P/V (show) Watery discharge P/V: sudden gush or constant leakage, amount, duration Confirm gestation: LMP,EDD Fetal movements Dilation of cervical os: cm Effacement of cervix: % of shortening/thinning Membrane: present/absent Presenting part: vertex/breech/others Station of presenting part in realtion to ischial spine Position of presenting part (denominator in relation to maternal pelvis) Clinical assessment of pelvis: diagonal conjugate, interspinous diameter, curvature of sacrum, suprapubic angle, transverse diameter of outlet, etc In postnatal cases Lochia: color, amount, smell Any vulva/vaginal swelling or tenderness with bluish discoloration of skin Perineal wound/episiotomy site: stitches, swelling, discharge, etc Internal examination not done unless indicated in cases like subinvolution, puerperal sepsis, suspected hematoma, retained pieces of placenta, post partum hemorrhage After history and examination a provisional diagnosis to be reached. In obstetric cases, diagnosis should be written completely including gravid, parity, gestational age, high risk conditions should be mentioned. In case of post natal cases: postnatal cases day and type of delivery should be mentioned Eg G3P1+1 AT 39 Weeks of pregenancy with previous LSCS in 1st stage of labor P2+0 AT 3RD day of peuperium after normal delivery with puerperal sepsis P1+0 at 2nd post op day of LSCS for fetal distress P3+0 at 1st day of forcep delivery for prolonged 2nd stage of labor with PPH
- 8. PROTOCOL FOR ANTENATAL CHECKUP Routine ANC investigations: 1. Hb%, Platelets 2. Blood grouping and Rh typing 3. VDRL (RPR) 4. HIV I and II 5. HBsAg 6. Random blood sugar 7. Urine routine USG scan for ANC patients: 1. Dating scan: 1st trimester 2. Anomaly scan: 18-20 weeks 3. 3RD scan at 38-40 weeks for fetal presentation, liqor volume (AFI), placental maturity grading, estimated fetal weight Medications during pregnancy 1. 1st trimester: Tab FOLIC ACID – 5mg OD Tab PERINORM 10 mg if needed 2. From 14 weeks onwards: Iron and calcium once daily, not to be taken at same time 3. Inj TT (0.5ml) im at 18 to 20 weeks – 1ST dose 2nd dose after 1 month 4. Deworming at the time of TT injection: Albendazole 400 mg single dose (at night) Follow up in ANC: 1. Every 4 weeks upto 28 weeks 2. Every 2 weeks upto 36 weeks 3. Every week upto 41 weeks Induction at 41 weeks ( after confirming the date) with: Cerviprime gel intracervical instillation at 2pm and 10pm or, Tab Misoprostol 24 μg at posterior fornix × 4 hourly after assessment × 3 doses Inj. Syntocinon drip at 6 am next morning depending on PV findings
- 9. Protocol for syntocinon: 2.5 units syntocinon in Inj. RL @ 10 drops/min, increase 1/2 hourly upto 40 drops/min depending on uterine contractions and FHS {good contraction pattern ( 3 contraction in 10 min each lasting > 40secs)} Do not give cerviprime, misoprostol or syntocinon in case of previous CS, malpresentation, grand multipara, suspected CPD or fetal distress PARTOGRAPH: Once the patient is in active labor i.e. cervical os= 4cm dilated, partograph should be filled. Vaginal examination should be done at 2 hr interval/SOS after that and each finding should be recoreded properly to assess the progress of labor. After delivery, partograph should be completed filling all the details of labor Management of 3RD stage of labor: After delivery of bay, palpate abdomen to exclude multiple pregnancy IV oxytocin 10 units (IU) Control cord traction to deliver the placenta Massage the uterus to maintain contraction Alternative uterotonics for management of PPH: Inj. Methergin 0.2mg im, Tab Misoprostol 600μg/800 μg) oral/rectal Inj. Carboprost 250 μg im should be available In cases of unusual excessive bleeding or if CCT fails to deliver placenta within half hour, inform senior on call immediately In case of prolonged 2ND stage of labor: inform senior on call after half hour to avoid delay in management Post delivery order: Watch out for PPH and hematoma Record vitals each 6 hours Pericare and light BD Exclusive breast feeding Analgesics SOS Counselling for family planning Discharge the patient after 24 hours, if everything is ok Continue iron and calcium for 6 weeks and PNC follow up in OPD after 6 weeks in normal delivery and 2 weeks in LSCS
- 10. Routine management of Post op patients: IV fluids and antibiotics and analgesics Inj. R/L + Inj DNS 6 pints over 24 hours Inj Pethidine 50mg + inj Phenargan 25 mg im 8 hourly Inj Diclofenac 75mg im SOS Inj Ranitidine 50 mg 8 hourly ANTIBIOTICS FOR LSCS and Laparotomy for ectopic pregnancy, ovarian cystectomy… Inj CEFTRIAXONE 1gm iv stat For TAH/VH Inj CIPROFLOXACIN 500mg IV BD Inj. METRON 500mg iv TDS Send post op Hb% next morning Iv drip omitted next morning after operation if patient stable Oral antibiotics to be continued for 7 days if needed Liquid diet on 1st day, soft diet on 2nd day and normal diet on 3rd day In abdominal surgeries including LSCS, dressing of wound done on 4th day and discharge if patient is stable In VH cases, catheter clamped on 3rd day, after 2nd sensation of bladder filling, catheter take out and patient discharged on 4th day after voiding of urine by herself All operated cases are followed up in OPD after 2 weeks or SOS MANAGEMENT OF HYPEREMESIS GRAVIDARUM: Investigations: Urine acetone DAILY till negative urine R/E Na/ K LFT Ultrasound scan for abdomen and pelvis to rule out multiple pregnancy, molar pregnancy and surgical conditions like cholelithiasis or other hepatic diseases Management: Nil per oral IV fluids: o Total 6 pints fluid : II pint 10% dextrose, II pint RL and II pint DNS o Inj B complex 1 ampule in I pint of 10% dextrose drip o Inj. Perinorm 10 mg IV 8 hourly o Inj. Ranitidine 50mg iv 8 hourly Once vomiting stops and urine acetone becomes negative patient is started with dry foods like biscuits, bread, etc Decrease drip to 6-8 hrly
- 11. Once tolerated then normal diet Ask patient about thirst, hunger, urine output during follow up history OUTPATIENT TREATMENT OF CASE OF VAGINITIS Tinidazole 2gm single dose Fluconazole 150mg single dose Clotrimazole ointment local application TDS Clotrimazole 200mg vaginal pessary for 3 nights or 100mg vaginal pessary for 6 nights OUTPATIENT TREATMENT OF CASE OF CERVICITIS Treatment same as vaginitis PLUS Azithromycin 500mg OD for 5 days Cefixime 400mg single dose OUTPATIENT TREATMENT OF CASE OF PID Treatment for cervicitis PLUS Drotin (antispasmodic) 40mg tds for 5 days IN-PATIENT TREATMENT OF CASE OF VAGINITIS Inj ceftriaxone 1gm iv 8 hourly till patient becomes afebrile and pain free for 24 hours and then o Cefixime 200mg iv BD for 7 days Inj Metron 500mg iv 8 hourly till patient becomes afebrile and pain free for 24 hours and then o Oral metron 400 mg 8 hourly for 7 days PLUS Azithromycin 500mg MANAGEMENT OF Rh negative pregnancy Investigations to be sent during ANC: 1. Husband’s blood group and Rh type 2. Anti D titre For primi at 28 weeks For multi at any trimester Repeat Anti D titre after one month Plan for induction of labor at 40 weeks of gestation, if spontaneous labor doesn’t take place then:
- 12. o At the time of delivery of baby, send cord blood from placental side of the cord for Hb% Blood grouping and Rh typing Total and direct bilirubin Direct Coombs test Injection anti-D-300 IU Intramuscular to be given to mother within 72 hours if direct coombs test is negative and baby’s blood group is Rh positive PREOPERATIVE INVESTIGATIONS FOR MAJOR SURGERIES: 1. Hb%, TC,DC Platelets 2. BT, CT 3. Blood grouping and Rh typing 4. Random blood sugar 5. Renal function test 6. HIV I & II 7. HBsAg 8. Urine r/e 9. Xray chest PA view 10. ECG 11. USG scan of Abdomen and Pelvis 12. Consult with anesthesiologist department night before surgery PRE OP PREPARATION OF PATIENT: Nil per oral after 10pm the day before operation Soap water enema at 6 am on the operative day Clean the operative area Arrange II pints of cross matched blood MANAGEMENT OF PRELABOUR RUPTURE OF MEMBRANE: Admit the patient, save pads, perform per speculum examination INVESTIGATIONS o CBC, CRP, High vaginal swab C/S Antibiotics o Erythromycin 500mg 6 hourly Syntocinon next morning at 6am MANAGEMENT OF PRE-ECLAMPSIA INVESTIGATIONS: Platelets
- 13. Coagulation profile: BT, CT Uric acid RFT LFT Urine R/E 24 hours urine albumin in case of severe pre eclampsia Medications Antihypertensive if BP > 140/90 mm of Hg, in more than one occasion or >160/100mg on one occasion start Capsule NIFEDIPINE 10mg orally 6-8 hourly MgSO4 as per national protocol in cases of sever pre-eclampsia or eclampsia Plan for termination of pregnancy (induction or LSCS) if uncontrolled. MANAGEMENT OF PEURPERAL PYREXIA: Investigations: CBC, High vaginal swab culture and sensivity, RFT, Blood culture, Urine routine and culture Ultrasound scan to rule out retained POC Medications: Inj ceftriaxone 1gm iv BD Inj. Metronidazole 500mg iv TDS Parenteral antibiotics for minimum 3 days or when patient is afebrile 48 hours switch to oral antibiotic If fever persists or USG shows RPOC, plan for exploration
