Jaundice in pregnancy
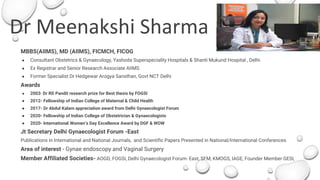
- 1. Dr Meenakshi Sharma MBBS(AIIMS), MD (AIIMS), FICMCH, FICOG ● Consultant Obstetrics & Gynaecology, Yashoda Superspeciality Hospitals & Shanti Mukund Hospital , Delhi ● Ex Registrar and Senior Research Associate AIIMS ● Former Specialist Dr Hedgewar Arogya Sansthan, Govt NCT Delhi Awards ● 2003- Dr RD Pandit research prize for Best thesis by FOGSI ● 2012- Fellowship of Indian College of Maternal & Child Health ● 2017- Dr Abdul Kalam appreciation award from Delhi Gynaecologist Forum ● 2020- Fellowship of Indian College of Obstetrician & Gynaecologists ● 2020- International Women’s Day Excellence Award by DGF & WOW Jt Secretary Delhi Gynaecologist Forum -East Publications in International and National Journals, and Scientific Papers Presented in National/International Conferences Area of interest - Gynae endoscopy and Vaginal Surgery Member Affiliated Societies- AOGD, FOGSI, Delhi Gynaecologist Forum- East, SFM, KMOGS, IAGE, Founder Member GESI,
- 2. Jaundice in Pregnancy Dr Meenakshi Sharma MBBS(AIIMS), MD (AIIMS), FICMCH, FICOG Senior Consultant Yashoda Superspeciality Hospital
- 3. Jaundice in pregnancy ● Clinical jaundice in 1:1000 pregnancy in India ● Incidence of total death due to jaundice in India 10-20%, 90% due to AVH ● Hepatitis is the most common and serious offending cause ● Mortality from infectious hepatitis is 3.5 fold higher in pregnancy when compared to non pregnant women ● Viral hepatitis accounts for 0.8-29.4% maternal deaths in various parts of India Arias High risk Pregnancy & Delivery, 4th ed 2015
- 4. Causes of Jaundice in Pregnancy ● Hepatitis ● Cholestasis ● Pregnancy related ● Hyperemesis ● Severe preeclampsia & eclampsia ● AFLP ● Cholelithiaisis ● Drugs ● Autoimmune hepatitis
- 5. Hepatitis in Pregnancy ● Specific hepatitis virus (A-E) ● Non A-E Viral hepatitis by Epstein Barr Virus, CMV, Echovirus, Yellow fever virus ● Non Viral hepatitis caused by bacterial(leptospirosis), parasitic (amoebiasis), drug toxicity and idiosyncratic reactions Fulminant hepatitis is more commonly seen in malnourished, immunocompromised pregnant women more commonly in third trimester and has high morbidity and mortality..
- 6. Feco -oral transmission - HAV and HEV ● More common in developing countries with crowding and poor sanitation ● Potential to cause epidemics ● HEV is endemic in India especially North and Central India and causes fulminant hepatitis Parenteral transmission through body fluids- HBV, HCV, HDV ● HBV and HCV both causes Chronic hepatitis, cirrhosis and HCC ● HCV causes chronic hepatitis in >50% of infection while only 10% of AVH due to HBV progress to chronic disease ● HDV only coexist with HBV as its incomplete virus, causes more severe disease Epidemiology
- 7. Clinical features Symptoms ● Asymptomatic ● Mild flu like symptoms ● Nausea, vomiting, Diarrhoea ● Fever usually rare ● Jaundice ● Pale stools, dark urine ● Right upper quadrant pain ● Hepatic encephalopathy Signs ● Icterus ● Palmar erythema, ● Ascites, ● Hepatic encephalopathy. ● MSOF
- 8. Clinical features HAV - mild asymptomatic disease usually unrecognised in pregnancy HBV - most common carrier state picked up on screening in pregnancy (4-6%) ● AVH in 25% of infected with mild flu like illness, jaundice and fever rare ● 90% of AVH resolve, 10% progress to chronic hepatitis, Cirrhosis and HCC ● Coinfection with HDV causes severe disease with recurrent hepatitis and cirrhosis and May progress to FHF HCV - mostly asymptomatic with raised ALT, more frequent in women with HIV ● HCV is not an important cause of AVH
- 9. Clinical features HEV - Primary cause of enterically transmitted NANB hepatitis ● Acute self limited disease like HAV ● Fulminant hepatitis occurs in 10% cases with 10-18% mortality ● No chronic carrier state ● Severe course in pregnancy ● Risk of Preterm labor, APH, PPH, maternal and perinatal mortality
- 10. Lab Evaluation Markers of hepatocyte metabolic/catabolic activities ● Bilirubin level ● Ammonia levels Markers of hepatocellular injury ● Aspartate aminotransferase (AST) ● Alanine aminotransferase (ALT) ● Alkaline phosphatase (ALP) Ratio of the ALT to ALP is < 2 , it indicates a cholestatic cause. Markers of hepatocyte synthetic function ● Prothrombin time (PT/PTT/INR) ● Albumin Specific viral markers USG Abdomen and Obstetrics
- 11. Appropriate Lab Evaluation - Hepatitis If ALT AST mildly elevated < x5 normal value ● Complete blood count, platelet count, AST, ALT, ALP, total Bilirubin, albumin, PT/INR, ● HAV Ag, IgM Ab, HBsAg, HBc Ab (IgM), HBsAb HBeAg, and HCV Ab, HEV Ag & Ab ● Iron panel (serum iron, total iron-binding capacity, serum transferrin saturation and serum ferritin) ● Ultrasound abdomen and Obstetrics If ALT AST severely elevated > x15 normal value or massive ALT >10.000 ● Ebstein-Barr virus, ● Cytomegalovirus, ● Ceruloplasmin (Wilson disease), ● Autoimmune markers (antinuclear antibodies, anti-smooth muscle antibodies, Anti- liver/kidney microsomal antibodies, IgG), ● Serum drug panel (including acetaminophen) and urine toxicology. ● Doppler abdominal ultrasound looking for vascular occlusion, eg. Budd-Chiari syndrome. American gastroenterology recommendations, Am J Gastroenterol. 2017
- 12. Lab Diagnosis HAV - Anti- HAV IgG & IgM HBV- HBsAg positive ● HBeAg & HBeAb reflects infectivity ● HBcAg & HBcAb - Core Ag and Ab reflects chronicity ● HBeAb positive and HBV DNA negative marks end of AVH even if HBsAg positive HCV- HCV viral RNA PCR, Anti HCV Ab positive is a marker of chronic infection HEV - HEV Ag, Anti HEV Ab
- 13. Vertical Transmission and Fetal effects HAV - not seen HBV - Transplacental transmission rare, mostly peripartum transmission ● HBeAg positive - fetal transmission 70-90% ● HBeAg negative, HBeAb negative - 25% ● HBeAg negative, HBeAb positive -12% ● 90% of Fetal transmission prevented by active and passive immunisation of newborn at birth ● Increased risk of prematurity and LBW neonates in AVH
- 14. Vertical Transmission and Fetal effects HCV - Vertical transmission similar to HBV ● Rate of transmission 3-6% but increases to 15% with HIV coinfection ● Rate of infection correlates with HCV viral load ● Breastfeeding doesn’t increase risk of transmission HEV - Vertical transmission occurs in 36% ● Fetal effects due to prematurity, LBW, Stillbirth and perinatal mortality
- 15. Burden of hepatitis E virus infection in pregnancy and maternofoetal outcomes: a systematic review and meta-analysis Prevalence of HEV in symptomatic women is 49.6%, in 52 studies (11,663 pregnant women) Vertical transmission in HEV 36.9%(13.3-64.2) HEV infection was associated with Maternal deaths (pooled OR 7.17; 3.32–15.47), Low birth weight (OR: 3.23; 1.71–6.10), Small for gestational age (OR: 3.63; 1.25–10.49), Preterm < 32 weeks (OR: 4.18; 1.23–14.20), and preterm < 37 weeks (OR: 3.45; 2.32– 5.13), Stillbirth (OR: 2.61; 1.64–4.14), Intrauterine deaths (OR: 3.07; 2.13–4.43), and not with miscarriage (OR: 1.74; 0.77–3.90) Bigna JJ, BMC Pregnancy Childbirth. 2020; 20: 426
- 16. Management - General measures Mild hepatitis - Symptomatic treatment ● Fluids, ● Antiemetic, ● Avoid hepatotoxic drugs and alcohol ● Screen for acute liver failure- encephalopathy, coagulopathy Acute Viral Hepatitis is usually self limiting, resolve in 2-4 weeks
- 17. Management HAV - Routine ANC care, HAV vaccine available ● Post exposure HAV vaccine (0,6 months) and HAV IG (0.02ml/kg) given HBV- Routine screening of antenatal patients and vaccinations of susceptible women, vaccinate seronegative antenatal women with husband HBsAg positive or high risk ● AVH managed by monitoring ALT and HBV DNA load- if HBV DNA > 106 copies/ml and high ALT- antiviral Rx with Lamivudine is safe effective and prevent perinatal transmission ● LSCS not recommended to decrease Fetal transmission ● Active and passive immunisation (HBV Immunoglobulin 0.06 ml/kg IM) to neonate within 12 hours of birth
- 20. Management HCV - No effective therapy, Mx supportive ● No vaccine available, Universal precautions to be followed ● Routine antenatal screening not recommended as no effective treatment and methods to prevent transmission available ● LSCS is not recommended to prevent Perinatal transmission HEV - Mild cases management supportive, Fulminant case requires intensive care ● No vaccine available ● Administration of immunoglobulin doesn’t prevent development of clinical disease
- 21. Acute Viral Hepatitis Causati ve Org. Transmis sion Incubatio n period C/F Diagnosis AVH in Pregnancy Management HAV RNA enterov irus Feco-oral 2-7 weeks Acute Viral hepatitis, mild self limiting, rarely FHF anti-HAV IgM 1:1000, no vertical transmission Immunoglobulin prophylaxis to mother and neonate HBV DNA Virus Body fluids 30-180 days AVH, Chronic Hepatits, cirrhosis, HCC 75% asymptomatic, 10% chronic hepatitis, Anti HBsAg IgG, IgM 1-2 :1000, 0.5-0.15% are carriers vertical transmission in 80% if untreated mostly peripartum, no transplacental transmission Prevention by vaccination, neonates HBV Immunoglobulin alongwith Vaccination HCV RNA virus Body fluids 15-150 days 80% asymptomatic, 50-80% chronic hepatitis or cirrhosis, HCC Anti- HCV IgG, IgM Vertical transmission 5%, 15% if coinfected with HIV FHF is rare more if coinfection or aplastic anemia No vaccine available No role of elective LSCS HDV Incomp lete virus Body fluids 35 days Coinfects with HBV 30% develop FHF,rapid progression to cirrhosis, mortality 25% HDV Ag No perinatal transmission HBV Vaccine HEV RNA virus Feco-oral 2-9 weeks Endemic in India, AVH, FHF in 10%, mortality 10-18% Anti-HEV IgM More severe disease in pregnancy, Vertical Transmission, prematurity, still birth, high morbidity and mortality No Vaccine
- 23. Definition Fulminant Hepatic Failure is defined as the rapid development of hepatocellular dysfunction, specifically coagulopathy and encephalopathy in a patient without known hepatic disease. Encephalopathy is the defining condition for FHF ● Acute onset, rapid progression to complications and worse predictions ● The basic pathology is massive necrosis, hepatic inflammation with the degeneration and destruction of hepatocytes and aggregation of macrophages
- 24. Causes of Acute Liver Failure in Pregnancy Pregnancy associated acute liver disease ● Pre-eclampsia/eclampsia with liver infarction ● HELLP syndrome ● Acute hepatic rupture ● Acute fatty liver of pregnancy (AFLP). Exacerbated by pregnant state ● Viral hepatitis ● Budd-Chiari syndrome (BCS) with portal vein thrombosis ● Gallstone disease. Unrelated to pregnant state ● Drug-induced liver disease ● Toxins/mushroom poisoning ● Shock ● Trauma ● Decompensation of pre-existent liver disease.
- 25. Pregnancy-associated acute liver disease (PAALD) Pregnancy induces certain physiological changes in the liver, which, if exaggerated, may result in pregnancy-associated acute liver disease (PAALD). PAALD has been proved to be associated with a worse prognosis and may require termination of pregnancy
- 26. FHF - Viral Hepatitis ● Hepatitis A, B, C, D, and E viruses, ● Herpes simplex virus, ● Cytomegalovirus, ● Epstein–Barr virus, Pregnant women were more susceptible for HEV infection and development of FHF. Rate and fatality increases with increasing gestational age
- 27. FHF - Indian Scenario ● 95% of FHF is virus-related, with 40% due to hepatitis E virus (HEV) and nearly 30% due to hepatitis B virus. ● More common in North and Central India. Mortality significantly low in South India due to high prevalence of protective anti HEV IgG ● Presence of encephalopathy on admission associated with high mortality ● Higher bilirubin level and low platelets predictive of higher mortality
- 28. FHF - Indian data AVH caused by HEV in 47.4%, (HAV-5.2%, HBV-7.2%, HCV-0%, non A-E 47.4%) in a study of 97 pregnant women with Hepatitis. ● 75% of FHF caused by HEV ● Mortality 24.7%(24/97) of AVH in pregnancy and all were due to FHF ● The mortality rate was 39.1% in HEV group and 11.7% in non HEV group ● 87.5% of women died undelivered Beniwal M, Indian J Med Microbiol Jul-Sep 2003;21(3):184-5.
- 29. FHF - HEV Prospective Observational study in 55 HEV IgM pregnant women ● 92% presented in the third trimester ● 77% of women had preterm labor ● 11% of them observed PPROM ● Maternal mortality about 5% ● Vertical transmission 28% A Study of Hepatitis E in Pregnancy: Maternal and Fetal Outcome. Prasad GS, Prasad S, Bhupali A, Patil AN, Parashar K. J Obstet Gynaecol India. 2016 Oct; 66(Suppl 1):18-23.
- 30. Mechanism of FHF in Pregnancy Pregnant women with HEV, particularly those in the second and third trimester, are at higher risk of poor materno-foetal outcomes ● Lower CD4/CD8 cells ratio ● Increased levels of steroid hormones ● Reduced progesterone receptor expression, ● Higher interleukin ● Viral load
- 31. FHF Hepatitis % incidence HAV 5.2% HBV 7.2% HCV 0% HEV 47.4% Non A-E 40.2% Beniwal M, Indian J Med Microbiol Jul-Sep 2003;21(3):184-5.
- 32. Acute liver failure in pregnancy: causative and prognostic factors. Shweta Sahai, Ravi Kiran. Saudi J Gastroenterol, Jan- Feb 2015;21(1):30-4 The pregnant women in whom no virus was detected could be suffering from PAALD (acute fatty liver, HELLP) or an infection from an unknown/undetected hepatotropic virus.
- 33. Acute liver failure in pregnancy: causative and prognostic factors. Shweta Sahai, Ravi Kiran. Saudi J Gastroenterol, Jan-Feb 2015;21(1):30-4
- 34. FHF perinatal outcome ● Spontaneous delivery/abortion occurred in 20 survivors (36.36%) and 8 nonsurvivors (61.53%) ● Majority of the pregnant women in ALF who died were undelivered (87.5%). ● Vertical transmission was seen in 3 out of the 10 newborns studied (transmission rate of 30%). This correlated very closely with the finding of Singh et al. and Beniwal et al. who found a vertical transmission rate of 33.33%. ● PAALD and viral hepatitis must be differentiated in pregnancy. It is recommended that PAALD should prompt early delivery. Shweta Sahai, Ravi Kiran. Saudi J Gastroenterol, Jan-Feb 2015;21(1) Beniwal M, Kumar A, Kar P, Jilani N, Sharma JB, Indian J Med Microbiol. 2003 Jul-Sep; 21(3):184-5. Devarbhavi H, Kremers WK, Dierkhising R, Padmanabhan L, J Hepatol. 2008 Dec; 49(6):930-5. Singh S, Mohanty A, Joshi YK, Deka D, Mohanty S, Panda SK, Indian J Pediatr. 2003 Jan; 70(1):37-9.
- 35. Management - General Considerations ● Multidisciplinary management by the intensivist, obstetrician, hepatologist, neonatologist, and if necessary, the transplant team. ● Early diagnosis and high index of suspicion in pregnant women with altered mental status, deranged liver function and coagulopathy ● Determining cause of liver failure challenging due to multiple etiology with overlapping features ● Maternal outcome takes precedence over fetal well-being
- 36. Management of FHF General management ● Prevention/treatment of cerebral oedema/intra-cranial hypertension ● Surveillance for infections and prompt antimicrobial treatment ● Correction of coagulopathy ● Maintenance of optimum haemodynamics ● Volume replacement ● Vasopressor support ● Renal perfusion. Correction of metabolic parameters ● Hypoglycaemia ● Dyselectrolytaemia ● Nutrition supplementation.
- 37. Management of Acute Liver Failure Aetiology specific treatment ● N acetylcysteine for paracetamol poisoning ● Mushroom poisoning-penicillin G and silymarin ● Herpes virus/varicella zoster-acyclovir ● Autoimmune hepatitis-corticosteroids (prednisone, 40–60 mg/day).
- 38. Acetaminophen toxicity N-Acetylcysteine - can be given oral or IV: ● 72-hour oral protocol - N-acetylcysteine oral: 140 mg/kg orally as a loading dose, followed by 70 mg/kg every 4 hours for a total of 17 doses ● or ● 20 hour IV protocol - N-acetylcysteine IV: 150 mg/kg intravenously over 60 minutes as a loading dose, followed by 50 mg/kg over 4 hours (12.5 mg/k/ per hour for 4 hrs), then 100 mg/kg over 16 hours (6.25 mg/kg per hour for 16 hours).
- 39. FHF Treatment ● Endotracheal intubation in patients with a GCS <8 and/or in the presence of active upper gastrointestinal bleeding. ● Management of respiratory failure and ALI with use of lung protective ventilation strategies; low tidal volume ∼6 mL/kg of predicted body weight, PEEP to maintain satisfactory oxygenation, and plateau pressures <30 cm/H2O to prevent further lung injury. ● Minimal sedatives, early mobilization and initiation of physical therapy to prevent weakness associated with immobility and critical illness. ● Patients may be hypotensive despite presence of a hyperdynamic state and being unresponsive to volume challenge. Vasopressors such as norepinephrine are titrated to achieve a mean arterial pressure of 65–70 mmHg. Vasopressin (or terlipressin) is norepinephrine-sparing in sepsis and appears to have a similar effect in patients with cirrhosis
- 40. Rx of Hepatorenal syndrome in ALF ● Volume expansion with albumin (1 g/kg maximum 100 g/day initial dose then followed by 20–40 g/day) ● Vasoconstrictors to decrease the serum creatinine to <1.2 mg/dL. Acceptable vasopresin - terlipressin, 0.5–1 mg given q4–6 h, increasing to 2 mg q4–6 h for up to 14 days. ● Therapeutic paracentesis for tense ascites which may result in the abdominal compartment syndrome which leads to renal, cardiovascular, and respiratory dysfunction. Large-volume paracentesis with concomitant albumin replacement at 6–8 g albumin per liter of ascites removed may be essential to reduce intra abdominal pressure. ● The mainstay of treatment of hepatic encephalopathy is use of lactulose and nonabsorbable antibiotics. The optimal dose of lactulose is not well established; however, titration to two to three semiformed stools per day is recommended.
- 41. Management - PAALD ● Hypertension associated PAALD - 25% of severe disease results in FHF, Maternal mortality 1% with treatment, Liver rupture 39% mortality ● The increased serum bilirubin and oliguria - predictors of mortality in PAALD, urgent delivery is indicated ● For foetal outcome, factors such as gestational age are more important than the severity of the syndrome. ● Infant morbidity and mortality ranges between 10% to 60% depending on the severity of maternal disease. ● Optimal treatment for maternal safety is an urgent delivery. If the pregnancy is >34 weeks gestation, immediate induction is recommended. If gestational age is between 24 and 34 weeks, corticosteroids are administered to accelerate foetal lung maturity in preparation for delivery 48 h later
- 42. Management - PAALD ● Subcapsular hematoma and liver rupture requires exploratory laparotomy with packing and has high mortality ● 0.3% Liver transplant occur in PAALD. The main indications for the liver transplant were liver failure, liver necrosis after rupture, and uncontrollable bleeding. ● An increasing trend toward conserving the pregnancy in contrast to expedite delivery as was practised before due to the availability of better intensive care and option for the liver transplant in face of severe and irreversible deterioration of liver functions. Acute liver failure in pregnancy: Challenges and management, Pandey C K et al, Indian J Anaesth. 2015 Mar; 59(3): 144–149
- 43. FHF - AFLP ● Incidence of 5/100,000, - abnormality in foetal fatty acid metabolism ● 18% maternal and 23% foetal mortality ● Maternal mortality is secondary to sepsis, renal failure, circulatory collapse, infection, pancreatitis or gastrointestinal bleeding ● Severe jaundice, coagulopathy, hepatic encephalopathy, ascites and hypoglycaemia in presence of a normal erythrocyte morphology and haptoglobin levels are pathognomonic of AFLP. ● Elevated AST > ALT, both <6 times above upper limit of normal, hyperbilirubinemia, hyperuricemia, high WBC > 15,000 cells/μL, hypoglycaemia, high ammonia and coagulopathy with or without DIC similar to sepsis ● Maternal stabilisation and Delivery is the only definitive therapy and has potential for full recovery ● Orthotopic LT (OLT) should be considered for those women with ALF, who manifest signs of irreversible liver failure despite delivery and aggressive supportive care.
- 44. Liver support Rx MARS - molecular absorbent recirculating system, reduced the levels of both water-soluble and albumin-bound substances and also improved the haemodynamics, clotting, hepatic, renal, neural and pulmonary function. It has been used as a life-saving measure in hepatic and renal dysfunction and oedema of the brain
- 45. FHF Budd Chiari Syndrome Hypercoagulability associated with protein C, protein S, antithrombin III deficiency as well as pregnancy itself poses risk factors for the development of this disease. Diagnosis by - Doppler ultrasonography of the right upper quadrant of the abdomen, followed by abdominal CT scanning. Venography is the ‘gold standard’ for diagnosis Management Anticoagulation with heparin unless contraindicated Surgical intervention to decompress the liver or transjugular intrahepatic portosystemic shunt placement in the presence of the gravid uterus can be technically difficult. LT has been shown to be effective in up to 88% of patients in combination with anticoagulation.
- 46. LIVER TRANSPLANTATION IN ACUTE LIVER FAILURE IN PREGNANCY Uncommon The indication of LT - HELLP syndrome are persistent bleeding despite surgical intervention, extensive liver necrosis or liver failure, AFLP. Cases have been reported of previable Liver transplantation that resulted in live-born infants post-viability. Case reports where postviable OLT was performed between 26 and 27 weeks gestation, associated with neonatal death 2-14 days after transplant, though case report of successful fetal outcome also reported where LT done at 27 weeks and LSCS done at 39 weeks and also in a case where combined LT and LSCS done at 32 weeks
- 47. Conclusion ● The availability of expert care in transplant surgery, hepatology, intensive care medicine, anaesthesiology, interventional radiology and neonatology must be considered when one is presented with a pregnant patient in ALF. ● Speedy diagnosis and treatment are crucial for management. ● In case of severe deterioration of hepatocellular function, LT is increasingly being considered as a treatment option especially in PAALD. ● When ALF complicates pregnancy, mortality approaches 40%, and LT is the viable alternative. The diagnosis should be considered early with consultation regarding termination of the pregnancy. ● Management protocols need to be individualised for each case keeping in mind the risk versus benefit to both the mother and the foetus.
- 49. Liver support devices are categorized into two main types: artificial livers, being acellular devices such as albumin dialysis and plasma- exchange/diafiltration, and bioartificial devices that contain cells from human, animal, or transformed sources. Early studies with both types of devices demonstrated biological effects (e.g., attenuation of systemic inflammatory response and improved biochemical profiles) but have failed to show a survival benefit. The liver support devices may improve quality of life and perhaps provide an economic benefit by reducing length of hospitalization. The determination of which patient benefits from liver support devices, or should be referred to early liver transplantation, and in which patient all treatment is futile awaits the results of future studies