Endotracheal intubation in oral & maxillofacial surgery
- 1. ENDOTRACHEAL INTUBATION IN ORAL & MAXILLOFACIAL SURGERY Dr. Padmasree Patowary
- 2. CONTENTS Introduction Historical prospective Indication and contraindication Armamentarium Procedure for Endotracheal Intubation Types of intubations I. Orotracheal intubation II. Nasoendotracheal intubation III. Retrograde intubation IV. Retromolar intubation V. Submental intubation VI. Fibroptic intubation Complications Conclusion.
- 3. Introduction Maintaining the airway is an essential step in oral and maxillofacial surgical cases, which are performed under general anesthesia or maxillofacial trauma. There are various techniques for maintaining the airway ranging from, head tilt – chin lift to surgical airway. Endotracheal intubation provides an artificial medium between the atmosphere and the patient’s trachea for the purpose of alveolar gas exchange or protection of the lungs from inappropriate substances.
- 4. Historical prospective Endotracheal intubation for the purpose of providing anaesthesia was first described by William Mac Ewan in 1878 when he passed a tube from the mouth into the trachea, using fingers as a guide in the conscious patient.
- 5. Routine To provide anaesthesia Emergency Airway obstruction Respiratory distress Oxygenation failure (hypoxia) Ventilation failure Mental status alteration Indications
- 6. Contraindication 1. Severe airway trauma or obstruction that does not permit safe way of an endotracheal tube. Emergency cricothyrotomy is indicated in such cases. 2. Cervical spine injury. 3. Mallampati Classification of class III / IV or other determination of potential difficult airway.
- 7. Intubation can be achieved in following ways: 1. After induction of general anaesthesia (by IV or inhalation method). a. Oral—orotracheal intubation. b. Nasal—nasotracheal intubation. 2. Awake intubation a. Blind oral b. Blind nasal c. Retrograde d. By use of fiberoptic scope. Procedure for Endotracheal Intubation
- 9. Upper Airway Anatomy • Anterior Nares • Vestibule • Mucosal Lining • Septum • Nasal conchea • Posterior Nares • Nasopharynx • Oropharynx • Pharynx • Larynx • Epiglottis • Vocal Folds • Glottis
- 10. Lower Airway Anatomy • Trachea • C-shaped cartilaginous rings • Carina • Right main bronchus • Left main bronchus • Bronchial Tree • Bronchioles • Alveolar ducts • Alveolar sacs • Alveoli – ̴300,000,000 • Capillaries
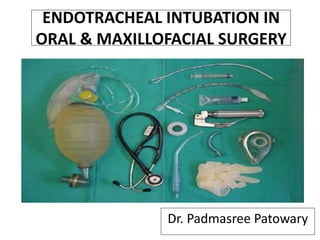
- 11. Armamentarium i. Anesthetic Mask ii. Laryngoscope iii. Endotracheal Tubes iv. Airways v. Laryngeal Mask Airway (LMA) vi. Magill’s forceps vii. Ambu Bag viii. Stylet
- 12. Mask is an essential part of any anaesthetic breathing system during the induction phase (beginning) of anaesthesia. A mask allows administration of gases from the breathing system, without introducing any invasive equipment (e.g. an endotracheal tube) into the patient’s airway. Face-masks are designed to fit the patient’s face perfectly without any leaks. • Parts: I. Connector or mount II. Body III. Edge or seal • Sizes: 1, 2, 3, 4, 5. Anesthetic Mask
- 13. Laryngoscope : handle and blade
- 14. LARYNGOSCOPIC BLADE • Macintosh (curved) blade (most popular) • Miller (straight) blade (useful for neonates and small children)
- 15. Laryngoscope is designed for doing direct laryngoscopy (directly viewing the vocal cords) and to pass an endo tracheal tube into the larynx under vision. • Parts: Handle, blade with light bulb. • Sizes (for the blades) Neonate (infant), Paediatric (child), adult and extra large.
- 16. Endotracheal tube is a specially designed tube with one end straight and the other being obliquely cut (beveled end). Beveled end enters the trachea. It is used for the surgical procedures in which it is not feasible to administer anaesthetic gases via mask, procedures which are long- lasting, procedures in which there are chances of having blood, secretions, pus, vomiting etc. in the oral cavity or where patient needs to be given muscle relaxants and controlled breathing. Endotracheal Tubes
- 17. It is always passed with direct laryngoscopy under vision after anaesthetizing the patient, except in cases, where patients are unable to open mouth, e.g. T.M. joint ankylosis or when a difficult intubation is expected. Age Weight (Inner) diameter (mm) New born 3 kg 2.5–3.0 0–6 months 3.5 kg 3.0–3.5 6–12 months 7 kg 3.5–4.0 1–3 years 10–12 kg 4.0–4.5 4–7 years 16–18 kg 5.0–5.5 8–10 years 24–30 kg 5.5–6.5 Adult female 7.0-7.5 Adult male 8.0-9.0
- 18. Types of endotracheal tube include 1. oral (south pole) or nasal (north pole) 2. cuffed or uncuffed 3. preformed (e.g. RAE (Ring, Adair, and Elwyn) tube 4. reinforced tubes 5. double-lumen endobronchial tubes.
- 19. The purpose of introducing an airway is to lift the tongue and epiglottis away from the posterior pharyngeal wall and prevent them from obstructing the space above the larynx. Airways I. Oropharyngeal (Oral) Airway (Placed from Lips to Pharynx) II. Nasopharyngeal (Nasal) Airway (Placed from the Nose to the Pharynx)
- 20. Oropharyngeal airway: In basic airway management, the oropharyngeal airway is used to provide a right airway to make possible for chest ventilation. In advanced airway management, it can be inserted following endotracheal intubation to act as a bite-block to protect the endotracheal tube. • Parts: Flange, bite portion, air/suction channel (curved portion) • Sizes: 1, 2, 3, 4.
- 21. Nasopharyngeal airway is a tube that is designed to be inserted into the nose to secure an open airway. When a patient becomes unconscious, the muscles in the jaw commonly relax and can allow the tongue to slide back and obstruct the airway. The purpose of the flared end is to prevent the device from becoming lost inside the patient's nose. •Parts: Flange or a movable disc attached to a tube • Sizes (diameter) — 7.0/7.5 for adult males — 6.5/7.0 for adult females — Same/one size smaller than an appropriate endotracheal tube for children
- 22. Laryngeal Mask Airway (LMA) Most popular supraglottic airway in emergency and short procedures. Consist of a tube with an inflatable cuff that is inserted into the pharynx . Very useful device in “can’t intubate / can’t ventilate” scenario. Parts: Mask, tube at an angle of 30 degrees, black line on tube to face upper incisors and pilot balloon. • Sizes: 1, 1.5, 2, 2.5, 3, 4, 5.
- 23. Designed by Dr Archie Brain in UK in 1981 and released in 1988
- 24. Indications: • When endotracheal intubation is not necessary or it is difficult Contraindications: • Non-fasted patients • Obstructive or abnormal lesions of the oropharynx
- 25. Advantages: • Allows rapid access • Does not require laryngoscope • Relaxants not needed • Provides controlled airway • Ventilation • Tolerated at lighter anesthetic planes Disadvantages: • Does not fully protect against aspiration in the non-fasted patient • Requires re-sterilization
- 26. Magill’s forceps is an instrument, which is most often used for guiding an endotracheal tube, from the pharynx into the larynx during nasal intubation. It is also used to pack the throat with a roller gauze during oral and pharyngeal surgery, to pick up a broken or dislodged tooth lying in the oral cavity or to pass a ryles (nasogastric) tube. It is L-shaped and it has no catch. It is available in two sizes—adult and paediatric. Magill’s forceps
- 27. •It is a combination of a self-inflating bag, a non- rebreathing valve and a facemask. • As it is useful for ventilating a patient in emergency situation, it should always be available in the operation theater as handy as possible. •If any problem occurs with anaesthesia machine or a breathing system, which cannot be diagnosed or corrected quickly, this bag will allow the user to ventilate the patient with room air (with or without oxygen) till the problem is solved. Ambu Bag
- 28. It is also useful and should be available during patient transport. It can also be used for administering anaesthesia in the absence of an anaesthesia machine, e.g., in rural set- up or field situations.
- 29. A stylet can be inserted inside an endotracheal tube to make it more rigid, or to change the shape of the tube. It is recommended that it can be used in all emergency intubations. In this way, if the shape of the tube needs to be modified, the stylet is already in place. The stylet should be lubricated before insertion into the endotracheal tube, so that it is easy to remove. Stylet
- 30. I. Orotracheal intubation II. Nasoendotracheal intubation III. Retromolar intubation IV. Submental intubation V. Retrograde intubation VI. Fibroptic intubation Types of Endotracheal intubation
- 31. Orotracheal Intubation • The oral route for intubating is preferred since it can usually be performed more rapidly and provides for better visualization. • In addition, the mouth can accommodate a larger tube than the nose.
- 32. INDICATIONS -Failure to oxygenate adequately. -Failure to ventilate adequately. -Failure of or need for airway maintenance or protection. -Expected need for intubation based on progression of underlying physiologic process. CONTRAINDICATIONS -Do Not Intubate (DNI) order -Partial tracheal transection -Difficult airway (relative)
- 34. Head positioning for tracheal intubation. A . Neutral position. B. Head elevated. C.“Sniffing” position with a flexed neck and extended head. Note that flexing the neck while extending the head lines up the various axes and allows direct laryngoscopy. D. Ramped position with elevation of the upper part of the back, neck, and head.
- 36. Trachlight • Light-guided intubation using the trachlight is a safe and gentle technique for both oral and nasal endotracheal tube placement and positioning . • A well defined circumscribed glow can be seen in the anterior neck when the endotracheal tube and light enter into the glottic opening.
- 38. Advantages • Minimal neck movement • Useful for laryngoscopy • Portable and inexpensive • Functional in bloody airway • Provides definitive airway Disadvantages • Blind technique • May damage airway • Expertise requires practice
- 39. Conformation • Chest lift • Movement of moisture column in ETT • Auscultation • Improvement and maintenance of SpO2 • Exhaled carbon dioxide
- 40. Nasoendotracheal intubation • Nasal intubation is applied for dental procedures performed in the hospital, dental office when possible. • Although many who provide anesthesia services are familiar and comfortable with nasal intubation techniques, some are uncomfortable because of lack of experience or fear of nasopharyngeal bleeding and trauma. • It has been observed from experiences in various settings that many approaches may be adapted to the technique of achieving nasal intubation
- 41. • Most commonly for dental procedures and intraoral (eg, mandibular reconstructive procedures) and oropharyngeal surgeries • Major maxillofacial surgeries • Securing the airway questionable cervical spine stability or severe degenerative cervical spine disease • Mass lesions or structural abnormalities • Limited mouth opening (eg : trismus). Indications
- 42. Absolute contraindications • Suspected inflammation of the epiglottis • Midface instability • Coagulopathy • Suspected fractures in base of the skull • Sleeping Apnea Relative contraindications • Large nasal polyps • Suspected nasal foreign bodies • Recent nasal surgery • Upper neck hematoma or infection • History of frequent episodes of epistaxis • Prosthetic heart valve (increased risk of bacteremia during the insertion) Contraindications
- 43. Technique of Nasotracheal Intubation Examine both nostrils to determine which is larger. Spray the nasal passages and back of the throat with an appropriate topical anesthetic and vasoconstrictor (neosynephrine) in order to numb the mucosa and reduce bleeding. Use of xylocaine jelly and a nasal airway before intubation, it may increase anesthesia and reduce bleeding. Remove the airway before intubation.
- 44. Pre-oxygenate the patient at 100% and keep the patient on Oxygen by a cannula in the mouth during the entire procedure. Check the balloon on an appropriately sized nasotracheal tube. Firmly seat the 15 mm adapter in the proximal end of the tube and lubricate the distal 4 cm with xylocaine jelly. Position the patients head in midline neutral position if possible. Patient may be sitting or supine position. Tell the patient that patient may feel like gagging or coughing when the tube is inserted. Advise the patient to resist gagging or coughing. Reassure and calm the patient.
- 45. With gentle pressure, insert the tube directed towards the occipital protuberance on the back of the skull with the bevel turned towards the nasal septum. Do not aim the tube up towards the vertex of the skull. If the tube will not pass on one side, try the other. Some resistance may be encountered when the tube reaches the posterior nasopharynx . At this point some gentle manipulation may need for pass the resistance. Turn the tube 1/4 turn after reaching the nasopharynx . Do not force it.
- 46. When the tube has reached the oropharynx at the back of the mouth, pay attention at the end of the tube for air moving in and out with each respiration. Gently but decisively push the tube further into the nostril and tube is enter into the trachea. Do not force the tube down as structures in the larynx. If properly placed, the tube will easily slip into the trachea. Confirm tube position in the same manner as for an orotracheal procedure. Control bleeding by gently pinching the nostrils around the tube. Secure tube with tape.
- 47. Retromolar Intubation Patients with panfacial trauma require specific considerations for securing airway intraoperatively. The necessity of intraoperative restoration of dental occlusion by maxillomandibular fixation (MMF) makes the presence of oral endotracheal tube unfeasible. Nasotracheal intubation is contraindicated in certain conditions – viz fracture of base of skull, fracture of naso-orbital-ethmoid complex, etc.In such cases, retromolar intubation, a non-invasive technique of securing airway in patients with panfacial trauma, avoids both submento-tracheal intubation and tracheostomy.
- 48. •Orotracheal intubation is done initially with a flexometallic tracheal tube using standard general anaesthesia technique. The aim is to place the orotracheal tube in the retromolar space (space behind the last upper and lower erupted molar teeth) . • The orotracheal tube is grasped with gloved fingers and is placed into the retromolar space. Technique
- 49. • The tube is then fixed by a wire ligature to the molar/premolar tooth. • The wire ligature is the same that is used for MMF. It fixes the retromolar tracheal tube with the tooth in a “figure of eight” fashion. • The retromolar tracheal tube allows adequate dental occlusion.
- 50. Advantages If retromolar intubation can be done with adequate dental occlusion, then tracheostomy and submento - tracheal intubation techniques can be avoided the. Disadvantages 1. In some patients, the retromolar space is not adequate. After retromolar placement of the tracheal tube dental occlusion is not possible. Therefore, intraoperative MMF cannot be done.
- 51. 2.The tracheal tube can interfere with the main surgical field that may be partially draped. 3.The tracheal tube can also interfere with positioning and application of dental fixation devices, especially in patients with bilateral maxillary/ mandibular fractures.
- 52. Submental Intubation Submental route of endotracheal intubation is a simple, safe and useful technique in maxillofacial trauma, where oral and nasal endotracheal intubation cannot be performed. It avoids the need for tracheostomy.
- 53. Technique • After a standard orotracheal intubation, a temporary draping of the mouth and chin was carried out. • Then, a 2-cm skin incision was made in the median region of the submental area, directly adjacent to the lower border of the mandible.
- 54. • The muscular layers (platisma and mylohyoid muscles) were traversed by blunt dissection using a Kelly forceps that was always in contact with the lingual cortex of the mandible. • The mucosal layer on the floor of the mouth was incised over the distal end of the forceps, and the forceps were then opened, creating a tunnel. During the dissection it is important that the width of the submental access should be sufficient to pass the tube without any interference.
- 55. •It is important to make sure that the tube has not been displaced during its passage through the submental tunnel. •After the surgery, the submental intubation was converted to an orotracheal intubation by replacing the tube in the mouth and carrying out extubation in the classical manner. Minimal scar postoperative.
- 56. •If the patient needed long-period postoperative ventilation, the orotracheal intubation was maintained until extubation was complete. •The suture was done with 5-0 nylon in the skin and 4-0 vycril in the internal layers.
- 57. Retrograde Intubation Ankylosing spondylitis (AS) patients are most challenging. Sound clinical judgment is critical for timing and selecting the method for airway intervention. The retrograde intubation technique is an important option when fiberoptic bronchoscope is not available, and other method is not applicable for gaining airway access for surgery in supaine position.
- 58. Indications 1. Facial Anomalies: a. Maxillary hypoplasia b. Mandibular hypoplasia c. Mandibular hyperplasia 2. Temporomandibular joint pathology: a. Ankylosis or reduced movment
- 59. 3. Anomalies of the mouth and tongue: a. Microstomia (burns, trauma scarring) b. Diseases of the tongue (burns, trauma, Ludwig angina) all lead to tongue swelling c. Tumors of the mouth and tongue (hemangioma, lymphangioma) d. Macroglossia (Down syndrome, hypothyroidism) 4. Problem with teeth (missing left upper incisors, protruding upper incisors)
- 60. Contraindication • Adequate mouth opening and easily performed orotracheal intubation • Relative contraindication: Systemic coagulopathy, infection in the skin overlying the cricothyroid membrane.
- 62. Fiberoptically guided tracheal intubation represents one of the most important advances in airway management to occur in the past thirty years. Perhaps its most important role is in management of the anticipated difficult airway. This is a situation in which the dangers of encountering the life- threatening "can't intubate, can't ventilate" situation can be avoided by placement of an endotracheal tube while the patient is awake. Fiberoptic Intubation
- 63. Indications: • Predictable difficult intubation (upper airway abnormality) • Cases where neck extension is not desirable • Nasal fiberoptic intubation in Oral Submucous Fibrosis Contraindications: • Inability to oxygenate • Major bleeding
- 64. 1. Eye piece 2. Diopter ring for focusing 3. Control lever 4. Working channel port 5. Body 6. Insertion cord 7. Light source 8. Suction valve and port Fiberoptic Bronchoscope
- 65. Technique • Oral or nasal route is preferable • Jaw thrust maneuver to improve visualization • After the broncoscope is lubricated and loaded with endotracheal tube it is introduced strictly in the midline following the base of the tongue, pass the uvula, behind epiglottis and between the vocal cords. • Once the carina is visualized endotracheal tube is introduced by rotating movement over the broncoscope.
- 67. Complications
- 68. 1) During intubation 2) During remained intubation 3) During extubation 4) After extubation
- 69. During intubation • Trauma to lip, tongue or teeth • Hypertension and tachycardia • Pulmonary aspiration. • Laryngospasm • Bronchospasm • Laryngeal edema • Arytenoid dislocation • Increased intracranial pressure • Spinal cord trauma in cervical spine injury
- 70. During remained intubation • Accidental extubation or endobronchial intubation. • Disconnection from breathing circuit Pulmonary aspiration. • Lip or nasal ulcer in case with prolong period of intubation. • Sinusitis in case with prolong nasoendotracheal intubation. • Esophageal intubation • Epistaxis
- 71. • Laryngospasm • Pulmonary aspiration • Edema of upper airway During extubation After extubation • Sore throat • Tracheal infection (Prolong intubation) • Laryngeal granuloma
- 72. Conclusion Airway management is the most important skill required of an anaesthesiologist and also for oral and maxillofacial surgeons. Endotracheal intubation is a skill based on the knowledge of airway anatomy, equipments for airway manipulation, also the use of pharmacological agents and experience.
- 73. REFERENCES • Miller’s Anesthesia, 7th Edition by Ronald D. Miller. • Clinical Anesthesiology, 4th Edition by G. Edward Morgan, Jr., Maged S. Mikhail, Michael J. Murray. • Bailey & Love’s Short Practice of Surgery, 25th Edition. • M Polansky. Airway Management: The Basics Of Endotracheal Intubation. The Internet Journal of Academic Physician Assistants 1996;(1):1. • Christopher Kabrhel, Todd W. Thomsen, Gary S. Setnik, Ron M. Walls. Orotracheal Intubation. N Engl J Med 2007;356:e15 • Endotracheal intubation: MedlinePlus Medical Encyclopedia • Textbook of OMFS , 3rd edition by Neelima malik • Malhotra N. Bhardwaj Chari P. :SUBMENTAL ENDOTRACHEAL INTUBATION:A USEFUL ALTERNATIVE TO TRACHEOSTOMYINDIAN JOURNAL OF ANAESTHESIA, OCTOBER 2002 2002; 46 (5) : 400-402
- 74. THANK YOU
Editor's Notes
- airway
- Armamentarium
- Class I: Pharyngeal pillars, entire palate, and uvula are visible. Class II: Pharyngeal pillars and soft palate are visible, with visualization of the uvula obstructed by the tongue. Class III: Soft palate is visible, but pharyngeal pillars and uvula are not visualized. Class IV: Only the hard palate is visible; the soft palate, pillars, and uvula are not visualized.
- Proper positioning of the clinician, patient, and assistant for tracheal intubation. The following points are demonstrated: the difficult airway cart is adjacent to the patient, the suction device is at the head of the bed, the patient is in the “sniffing position” with the occiput elevated and the clinician’s right hand ready for additional adjustment if necessary, the bed is elevated and the clinician is at the appropriate distance from the patient, and the laryngoscope handle is angled at 45 degrees.
- Eye piece: Can be attached to a camera for display on screen. fiberoptic scopes have an eye piece; video scopes do not. Diopter ring for focusing Control lever: Controls the tip. Only permits movement in a vertical plane. Two wires extend from the handle to the tip in the insertion cord. Moving the lever down, moves the tip up and moving the lever up, points the tip down. Side to side movement is accomplished by rotation of the body of the bronchoscope with the operator's wrist and shoulder. Working channel port: For suction, instillation of local anesthetic, oxygen delivery. Body: Incorporates the eye piece, diopter ring, control level and working channel. Grasped by the operators non-dominant hand. Insertion cord: Contains fiberoptic bundle for light and image transmission, tip bending control wires and working channel. Average length 600mm (range 500 – 650mm). Light source: Can be a portable battery powered source or via a cable. Light source may be halogen, incandescent or LED. Suction valve and port
