NATIONAL PREVENTION STRATEGY 2011
- 1. National Prevention Strategy America’s Plan for Better Health and Wellness June 16, 2011
- 2. 2
- 3. National Prevention Message from the Chair of the National Strategy Prevention, Health Promotion, and Public Health Council As U.S. Surgeon General and Chair of the National Prevention, Health Promotion, and Public Health Council (National Prevention Council), I am honored to present the nation’s first ever National Prevention and Health Promotion Strategy (National Prevention Strategy). This strategy is a critical component of the Affordable Care Act, and it provides an opportunity for us to become a more healthy and fit nation. The National Prevention Council comprises 17 heads of departments, agencies, and offices across the Federal government who are committed to promoting prevention and wellness. The Council provides the leadership necessary to engage not only the federal government but a diverse array of stakeholders, from state and local policy makers, to business leaders, to individuals, their families and communities, to champion the policies and programs needed to ensure the health of Americans prospers. With guidance from the public and the Advisory Group on Prevention, Health Promotion, and Integrative and Public Health, the National Prevention Council developed this Strategy. The National Prevention Strategy will move us from a system of sick care to one based on wellness and prevention. It builds upon the state-of-the-art clinical services we have in this country and the remarkable progress that has been made toward understanding how to improve the health of individuals, families, and communities through prevention. The National Prevention Strategy encourages partnerships among Federal, state, tribal, local, and territorial governments; business, industry, and other private sector partners; philanthropic organizations; community and faith-based organizations; and everyday Americans to improve health through prevention. For the first time in the history of our nation, we have developed a cross-sector, integrated national strategy that identifies priorities for improving the health of Americans. Through these partnerships, the National Prevention Strategy will improve America’s health by helping to create healthy and safe communities, expand clinical and community- based preventive services, empower people to make healthy choices, and eliminate health disparities. We know that preventing disease before it starts is critical to helping people live longer, healthier lives and keeping health care costs down. Poor diet, physical inactivity, tobacco use, and alcohol misuse are just some of the challenges we face. We also know that many of the strongest predictors of health and well-being fall outside of the health care setting. Our housing, transportation, education, workplaces, and environment are major elements that impact the physical and mental health of Americans. This is why the National Prevention Strategy helps us understand how to weave prevention into the fabric of our everyday lives. The National Prevention Council members and I are fully committed to implementing the National Prevention Strategy. We look forward to continuing our dialogue with all stakeholders as we strive to ensure that programs and policies effectively help us accomplish our vision of a healthy and fit nation. Regina M. Benjamin, MD, Surgeon General Chair of the National Prevention, Health Promotion, and Public Health Council 3
- 4. National Prevention, Health Promotion, and Public Health Council Members • Surgeon General Regina M. Benjamin, Council Chair • Secretary Kathleen Sebelius, Department of Health and Human Services • Secretary Tom Vilsack, Department of Agriculture • Secretary Arne Duncan, Department of Education • Chairman Jon Leibowitz, Federal Trade Commission • Secretary Ray LaHood, Department of Transportation • Secretary Hilda L. Solis, Department of Labor • Secretary Janet A. Napolitano, Department of Homeland Security • Administrator Lisa P. Jackson, Environmental Protection Agency • Director R. Gil Kerlikowske, Office of National Drug Control Policy • Director Melody Barnes, Domestic Policy Council • Assistant Secretary-Indian Affairs Larry Echo Hawk, Department of the Interior • Acting Chief Executive Officer Robert Velasco II, Corporation for National and Community Service • Secretary Robert M. Gates, Department of Defense • Secretary Shaun Donovan, Department of Housing and Urban Development • Attorney General Eric H. Holder, Jr., Department of Justice • Secretary Eric K. Shinseki, Department of Veterans Affairs • Director Jacob J. Lew, Office of Management and Budget 4
- 5. Table of Contents Message from the Chair of the National Prevention, Health Promotion, and Public Health Council...........................3 National Prevention, Health Promotion, and Public Health Council .........................................................................4 Table of Contents ..................................................................................................................................................5 Introduction .........................................................................................................................................................6 National Leadership ..............................................................................................................................................8 Partners in Prevention ...........................................................................................................................................9 Strategic Directions and Priorities ........................................................................................................................11 Strategic Directions Healthy and Safe Community Environments..................................................................................................14 Clinical and Community Preventive Services ..................................................................................................18 Empowered People ......................................................................................................................................22 Elimination of Health Disparities ...................................................................................................................25 Priorities Tobacco Free Living......................................................................................................................................28 Preventing Drug Abuse and Excessive Alcohol Use .......................................................................................31 Healthy Eating .............................................................................................................................................34 Active Living ................................................................................................................................................38 Injury and Violence Free Living .....................................................................................................................41 Reproductive and Sexual Health ...................................................................................................................44 Mental and Emotional Well-being .................................................................................................................48 Appendices Appendix 1: Economic Benefits of Preventing Disease ......................................................................................51 Appendix 2: National Prevention Strategy Indicators .......................................................................................52 Appendix 3: Stakeholder Outreach and Input ...................................................................................................61 Appendix 4: Advisory Group on Prevention, Health Promotion, and Integrative and Public Health ....................62 Appendix 5: Justification for Evidence-Based Recommendations ........................................................................63 Appendix 6: References for the Key Documents ................................................................................................82 Appendix 7: End Notes ...................................................................................................................................87 5
- 6. Introduction The strength and ingenuity of America’s people and communities have driven America’s success. A healthy and fit nation is vital to that strength and is the bedrock of the productivity, innovation, and entrepreneurship essential for our future. Healthy people can enjoy their lives, go to work, contribute to their communities, learn, and support their families and friends. A healthy nation is able to educate its people, create and sustain a thriving economy, defend itself, and remain prepared for emergencies. The Affordable Care Act, landmark health legislation passed basic needs and providing information about personal health and in 2010, created the National Prevention Council and called health care can empower people to make healthy choices, laying for the development of the National Prevention Strategy to a foundation for lifelong wellness. realize the benefits of prevention for all Americans’ health. The National Prevention Strategy is critical to the prevention focus Preventing disease requires more than providing people with of the Affordable Care Act and builds on the law’s efforts to information to make healthy choices. While knowledge is critical, lower health care costs, improve the quality of care, and provide communities must reinforce and support health, for example, by coverage options for the uninsured. making healthy choices easy and affordable. We will succeed in creating healthy community environments when the air and water Preventing disease and injuries is key to improving America’s are clean and safe; when housing is safe and affordable; when health. When we invest in prevention, the benefits are broadly transportation and community infrastructure provide people shared. Children grow up in communities, homes, and families with the opportunity to be active and safe; when schools serve that nurture their healthy development, and people are children healthy food and provide quality physical education; and productive and healthy, both inside and outside the workplace. when businesses* provide healthy and safe working conditions Businesses benefit because a healthier workforce reduces long- and access to comprehensive wellness programs. When all term health care costs and increases stability and productivity. sectors (e.g., housing, transportation, labor, education, defense) Furthermore, communities that offer a healthy, productive, stable promote prevention-oriented environments and policies, they all workforce can be more attractive places for families to live and contribute to health. for businesses to locate. The National Prevention Strategy builds on the fact that lifelong Although America provides some of the world’s best health care health starts at birth and continues throughout all stages of life. and spent over $2.5 trillion for health in 2009, the U.S. still Prevention begins with planning and having a healthy pregnancy, ranks below many countries in life expectancy, infant mortality, develops into good eating and fitness habits in childhood, and many other indicators of healthy life.1 Most of our nation’s is supported by preventive services at all stages of life, and pressing health problems can be prevented. Eating healthfully promotes the ability to remain active, independent, and involved and engaging in regular physical activity, avoiding tobacco, in one’s community as we age. Students who are healthy and excessive alcohol use, and other drug abuse, using seat belts, and fit come to school ready to learn; employees who are free from receiving preventive services and vaccinations are just a few of mental and physical conditions take fewer sick days, are more the ways people can stay healthy. Health is more than merely the productive, and help strengthen the economy; and older adults absence of disease; it is physical, mental, and social well-being.2 who remain physically and mentally active are more likely to live Investments in prevention complement and support treatment independently.4 and care. Prevention policies and programs can be cost-effective, reduce health care costs, and improve productivity (Appendix 1). To ensure that all Americans share in the benefits of prevention, The National Prevention Strategy’s core value is that Americans the National Prevention Strategy includes an important focus can live longer and healthier through prevention. on those who are disproportionately burdened by poor health. In the United States, significant health disparities exist and Many of the strongest predictors of health and well-being these disparities are closely linked with social, economic, and fall outside of the health care setting. Social, economic, and environmental disadvantage (e.g., lack of access to quality environmental factors all influence health.3 People with a quality affordable health care, healthy food, safe opportunities for education, stable employment, safe homes and neighborhoods, physical activity, and educational and employment opportunities). and access to high quality preventive services tend to be healthier throughout their lives and live longer. When organizations, whether they are governmental, private, or nonprofit, succeed in meeting these basic needs, people are more likely to exercise, eat healthy foods, and seek preventive health services. Meeting * Consistent with existing laws 6
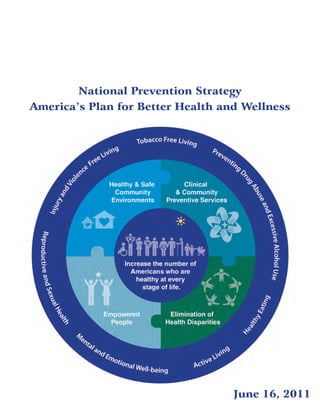
- 7. National Prevention Strategy The National Prevention Strategy leading causes of preventable death and major illness. The seven The National Prevention Strategy aims to guide our nation in the Priorities are most effective and achievable means for improving health and well-being. The Strategy prioritizes prevention by integrating • Tobacco Free Living recommendations and actions across multiple settings to improve • Preventing Drug Abuse and Excessive Alcohol Use health and save lives. • Healthy Eating • Active Living The National Prevention Strategy’s vision is Working • Injury and Violence Free Living together to improve the health and quality of life for • Reproductive and Sexual Health individuals, families, and communities by moving the • Mental and Emotional Well-Being nation from a focus on sickness and disease to one based on prevention and wellness. Moving Forward National leadership is critical to implementing this Strategy. This leadership includes aligning and focusing Federal prevention This Strategy envisions a prevention-oriented society where all efforts. However, the Federal government will not be successful sectors recognize the value of health for individuals, families, acting alone. Partners in prevention from all sectors in American and society and work together to achieve better health for all society are needed for the Strategy to succeed. All of us must Americans.. act together, implementing the Strategic Directions and Priorities, so that all Americans can live longer and healthier at every stage The National Prevention Strategy’s overarching goal is of life. Increase the number of Americans who are healthy at every stage of life. This Strategy focuses on both increasing the length of people’s lives and ensuring that people’s lives are healthy and productive. Currently Americans can expect to live 78 years, but only 69 of these years would be spent in good health.5 Implementing the National Prevention Strategy can increase both the length and quality of life. To monitor progress on this goal, the Council will track and report measures of the length and quality of life at key life stages (Appendix 2 for baselines and targets). To realize this vision and achieve this goal, the Strategy identifies four Strategic Directions and seven targeted Priorities. The Strategic Directions provide a strong foundation for all of our nation’s prevention efforts and include core recommendations necessary to build a prevention-oriented society. The Strategic Directions are • Healthy and Safe Community Environments: Create, sustain, and recognize communities that promote health and wellness through prevention. • Clinical and Community Preventive Services: Ensure that prevention-focused health care and community prevention efforts are available, integrated, and mutually reinforcing. • Empowered People: Support people in making healthy choices. • Elimination of Health Disparities: Eliminate disparities, improving the quality of life for all Americans. Within this framework, the Priorities provide evidence-based recommendations that are most likely to reduce the burden of the 7
- 8. National Leadership National leadership is critical to support our nation’s focus on prevention, catalyze action across society, and implement the Strategic Directions and Priorities of the National Prevention Strategy. The National Prevention Council, created through the Affordable Care Act, comprises 17 Federal departments, agencies and offices and is chaired by the Surgeon General. The National Prevention Council developed the Strategy with input from the Prevention Advisory Group, stakeholders, and the public (Appendix 3). The Council will continue to provide national leadership, engage a diverse array of stakeholders, facilitate coordination and alignment among Federal departments, agencies, and offices and non-Federal partners, champion the implementation of effective policies and programs, and ensure accountability. Provide National Leadership policy and program recommendations as new evidence becomes The National Prevention Council provides coordination and available. The Council will review new and emerging data and leadership at the Federal level and identifies ways that agencies can evidence, prioritizing our nation’s health needs and providing work individually, as well as together, to improve our nation’s health. information to the President and Congress concerning the most The Council helps each agency incorporate health considerations pressing health issues confronting the United States. into decision making, enhances collaboration on implementing prevention and health promotion initiatives, facilitates sharing of best Ensure Accountability – Annual Status practices, and, as appropriate, coordinates guidance and funding Report streams. The Council will identify specific, measurable actions and The National Prevention Council will track progress in timelines to carry out the Strategy, and will determine accountability implementing the National Prevention Strategy, report on for meeting those timelines within and across Federal departments successes and challenges, and identify actions that are working, and agencies. as well as areas where additional effort is needed. The Strategy contains metrics that will be used to measure progress. Key Engage Partners indicators are identified for the overarching goal, the leading The Council will ensure ongoing engagement of partners from causes of death, and each of the Strategic Directions and all parts of society to understand and act upon advancements Priorities. Each year, the National Prevention Council will deliver and developments that may affect health and wellness through an Annual Status Report to the President and Congress. prevention. Partners are necessary to implement the Strategy at the national, state, tribal, local, and territorial levels. The Council will The Prevention Advisory Group foster partnerships, identify areas for enhanced coordination and The Advisory Group on Prevention, Health Promotion, and alignment, and disseminate best practices. Integrative and Public Health (Prevention Advisory Group), also created by the Affordable Care Act, brings a non- Align Policies and Programs Federal perspective to the Strategy’s policy and program Aligning policies and programs at the national, state, tribal, recommendations and to its implementation. The Presidentially local, and territorial levels can help ensure that actions are appointed Prevention Advisory Group (Appendix 4) will assist synergistic and complementary. When all sectors are working in the implementation of the Strategy, working with partners toward common prevention priorities, improvements in health throughout the nation. The Prevention Advisory Group will advise can be amplified. The National Prevention Council will work to the National Prevention Council in developing public, private, identify and facilitate the sharing of best practices to support the and nonprofit partnerships that will leverage opportunities to alignment of actions with what has been shown to be effective. improve our nation’s health. The Prevention Advisory Group will also continue to develop and suggest policy and program Assess New and Emerging Trends and recommendations to the Council. Evidence The prevention landscape continuously evolves as scientific evidence, new plans and reports, new legislation, and innovative partnerships emerge. The Strategy will adapt its approaches as new information becomes available. The National Prevention Council will gather input to identify promising practices and innovative approaches to prevention and integrative health. The Council will maintain close ties to prevention practice and research, updating 8
- 9. National Prevention Partners in Prevention Strategy Aligning and coordinating prevention efforts across a wide range of partners is central to the success of the National Prevention Strategy. Engaging partners across disciplines, sectors, and institutions can change the way communities conceptualize and solve problems, enhance implementation of innovative strategies, and improve individual and community well-being. Who are the Partners in Prevention? Employer Employers have the ability Building a Prevention The Federal government alone cannot create healthier communities. to implement policies and Foundation through State, tribal, local, and territorial governments, businesses, health programs that foster health, Partnerships care, education, and community and faith-based organizations are all wellness, and safety among Improving the health of essential partners in this effort. their employees. Evidence- our nation’s workforce is based work-site employee good for both employees Roles that Partners Play and employers – it wellness and safety policies and A wide range of actions contribute to and support prevention, programs can reduce health improves employee ranging, for example, from a small business that supports risks and improve the quality productivity, reduces evidence-based workplace wellness efforts, to a community-based of life for millions of workers in health care expenditures, organization that provides job training for the unemployed, to the United States. For example, and encourages economic the parent of young children who works to provide healthy foods employers can provide tailored, growth. Employers can and ensure they receive appropriate preventive services. Partners confidential counseling to implement policies and play a variety of roles and, at their best, are trusted members of promote life skills, combat programs to improve the the communities and populations they serve. Opportunities for depression, address substance health of their workers, for prevention increase when those working in housing, transportation, use problems, and enhance example, by protecting their education, and other sectors incorporate health and wellness into overall emotional well-being workers from illness and their decision making. The following roles exemplify opportunities for employees. injury, ensuring access to that partners can take to support prevention: healthy foods, and providing Funder health coverage for clinical Policy Maker preventive services. Funding for research, programs, Individuals, organizations, and communities have a role in operations, and infrastructure developing, implementing, and enforcing policies, laws, and (e.g., roads) can be used to improve prevention. Organizations regulations within their jurisdictions, whether they are states, cities, that provide financial support can encourage funding recipients communities, work sites, schools, or recreation areas. Organizations to adhere to health principles and standards, leverage cross-sector can explicitly consider the potential health impact of policy options collaboration, and support development of healthy communities. and choose to implement those policies that improve health. For For example, state, tribal, local, and territorial governments can example, a metropolitan planning organization can institutionalize incorporate recommendations for physical activity and standards for the use of health criteria when making planning decisions on land healthy eating into performance standards for schools and child care use and design to provide opportunities for safe physical activity. centers. Purchaser Individuals, agencies, and organizations purchase various goods Data Collector and Researcher Data and research can be used to strengthen implementation of and services, such as food, vehicles, health insurance, and supplies, the National Prevention Strategy. For example, a university can and some finance the construction of infrastructure projects, such as help demonstrate the business case for prevention and share buildings, housing, and roads. They can use their purchasing power these findings with corporate decision makers (e.g., board chairs, to promote health and wellness. For example, businesses can adopt corporate officers). Further, researchers can work with communities policies to procure healthy foods and build healthier environments by providing data that present a comprehensive community for their workers and customers. profile (e.g., community health status and data on transportation, recreation, labor, environment, and education), helping identify evidence-based strategies, and measuring progress. 9
- 10. Partners in Prevention Health Care Provider Communicator and Educator Individuals and organizations that deliver health care services Individuals and communities provide and receive information can implement policies and systems to support the delivery of through many sources. Advertising, educational campaigns, high-impact clinical preventive services and enhance linkages informational websites, and trainings can raise awareness, between clinical and community prevention efforts. For example, provide people with knowledge and skills, and create supportive a health care system can adopt a decision support system that environments to help people make healthy decisions. prompts clinicians to deliver appropriate clinical preventive services to patients. PROJECT HIGHLIGHT: Incorporating Health in Regional Transportation Planning: Nashville, Tennessee Recognizing the relationship between the built environment, transportation, and health, the Nashville Area Metropolitan Planning Organization adopted a set of guiding principles, goals, and objectives to help the region pursue quality growth as a central part of its 25-year regional transportation plan. Emphasizing mass transit, active transportation (e.g., biking, walking), and preservation and enhancement of roadways, the plan incorporates health considerations into infrastructure project selection. Sixty percent of the selection criteria are related to health, safety, congestion reduction, and active transportation, which has resulted in the inclusion of sidewalks, bicycle lanes, or shared-use lanes in 70 percent of funded roadway projects (up from 2 percent). The plan also reserves a minimum of 25 percent of Federal Surface Transportation Project dollars for active transportation. 10
- 11. National Prevention Strategic Directions and Priorities Strategy We know a great deal about how to improve the health of the nation; decades of research and practice have built the evidence base and identified effective prevention approaches. Improving socioeconomic factors (e.g., poverty, education) and providing healthful environments (e.g., ensuring clean water, air and safe food, designing communities to promote increased physical activity) reinforce prevention across broad segments of society. Broad-based changes that benefit everyone in a community should be supplemented by clinical services that meet individual health needs (e.g., immunization, colonoscopy, tobacco cessation counseling, blood pressure and cholesterol monitoring and control). Through health promotion, education, and counseling, we can provide people with the knowledge, tools, and options they need to make healthy choices. Strategic Directions and resources, they are empowered to make healthier choices. The National Prevention Strategy identifies four Strategic Efforts to educate and motivate people to make healthy choices Directions. These Strategic Directions are the foundation for all should occur across the lifespan, with a particular emphasis on prevention efforts and form the basis for a prevention-oriented ensuring that young people are provided with the knowledge, society. Each Strategic Direction can stand alone and can guide skills, and opportunities they need to allow them to become actions that will demonstrably improve health. Together, the healthy adults. In addition, we should provide knowledge and Strategic Directions create the web needed to fully support opportunities that support the unique needs of our growing older Americans in leading longer and healthier lives. adult population. Healthy and Safe Community Environments: Create, Elimination of Health Disparities: Eliminate disparities, sustain, and recognize communities that promote health and wellness improving the quality of life for all Americans. All Americans should through prevention. Many elements of our communities affect have the opportunity to live long, healthy, independent, and health directly and also influence individuals’ health-related productive lives, regardless of their race or ethnicity; religion; choices. A healthy community environment can help make socioeconomic status; gender; age; mental health; cognitive, healthy choices easy and affordable. Many factors influence sensory, or physical disability; sexual orientation or gender individual choices, including the availability of resources to identity; geographic location; or other characteristics. In the meet daily needs (e.g., educational and job opportunities, United States, health disparities are often closely linked with safe and affordable housing, healthy and affordable foods); social, economic, or environmental disadvantage. Clear evidence community structures (e.g., accessible and safe buildings, parks, exists that with appropriate focus and investment, health transportation); and the natural environment (e.g., absence of disparities can be eliminated while simultaneously improving the toxic substances and other physical hazards). Federal, state, tribal, health of all Americans. local, and territorial policies that improve these factors within communities are often interrelated. Priorities Americans aspire to live long, healthy, and productive lives; Clinical and Community Preventive Services: Ensure however, obesity, tobacco use, misuse of alcohol and other that prevention-focused health care and community prevention efforts substances, and community stressors (e.g., job and home losses, are available, integrated, and mutually reinforcing. The provision of discrimination, family separations, and violence) are serious evidence-based clinical and community preventive services and threats to health. In addition, too many Americans do not receive the integration of these activities are central to improving and the preventive services that help maintain health, prevent or enhancing physical and mental health. Certain clinical preventive delay the onset of disease, and reduce health care costs. Each services have proven to be both effective and cost-saving through year, injuries and chronic diseases such as heart disease, cancer, decades of practice and research; The Affordable Care Act reduces and diabetes are responsible barriers to people receiving many clinical preventive services. for millions of premature Clinical preventive services can be supported and reinforced by deaths among Americans. In Together, chronic illnesses community prevention efforts that have the potential to reach 2005, 133 million Americans (e.g., cancer, obesity, large numbers of people. – almost one in two adults – depression) cause had at least one chronic illness. Americans to miss 2.5 Empowered People: Support people in making healthier Furthermore, injuries are the billion days of work each choices. Although policies and programs can make healthy options leading cause of death among year, resulting in lost available, people still need to make healthy choices. When people infants, youth, and young productivity totaling more have access to actionable and easy-to-understand information adults.6 Most of these early than $1 trillion.7 11
- 12. Strategic Directions and Priorities deaths can be avoided, adding extra years of productivity and Five Causes Account for the Majority of Deaths enjoyment for millions of people. 5 leading causes (66% of all deaths): The Strategy’s seven Priorities are designed to improve health and Heart disease wellness for the entire U.S. population, including those groups Cancer 27% All other causes disproportionately affected by disease and injury. 34% Chronic lower respiratory disease • Tobacco Free Living Stroke • Preventing Drug Abuse and Excessive Alcohol Use Unintentional injuries • Healthy Eating 23% • Active Living 5% • Injury and Violence Free Living 5% • Reproductive and Sexual Health 6% • Mental and Emotional Well-Being Source: National Vital Statistics Report, CDC, 2008 Recommendations and Actions The Strategy provides evidence-based recommendations for In addition to the recommendations, the Strategy identifies All other causes improving health and wellness and addressing leading causes of actions that the Federal government will take and that disability and death. Recommended policy, program, and systems partners can take to promote health and wellness. The approaches are identified for each Strategic Direction and Priority. “Federal government will” statements identify actions that the Preference has been given to efforts that will have the greatest National Prevention Council departments will take to guide the impact on the largest number of people and can be sustained implementation of the Strategy. These statements represent over time. Each recommendation is based on the best recent both new and existing initiatives. Some may include newly scientific evidence (Appendix 5). incorporating prevention into policies and regulations, while others may incorporate or enhance prevention as part of existing Current evidence for prevention is strong, and when effective programs. Whether in new or existing initiatives, all actions strategies are implemented they drive significant improvement in will be subject to the annual budget processes that require the public’s health. Effective types of strategies fall into five major balancing priorities within available resources. The “partners can” categories: policy, systems change, environment, communications statements identify actions that different partners can voluntarily and media, and program and service delivery. Policy, system pursue to promote prevention. These evidence-based options change, and environmental strategies can be very cost-effective draw from a variety of sources, including public input. ways to improve the public’s health. There are, however, areas where additional effective strategies are needed. Future Measuring Progress research and evaluation, including well designed trials for many The Strategy includes key indicators for a) the overarching goal, complementary and alternative medicine therapies, will be critical b) the leading causes of death, and c) each Strategic Direction to addressing unmet prevention and wellness needs, and new and Priority. These indicators will be used to measure progress in evidence-based strategies will be incorporated as they emerge. prevention and to plan and implement future prevention efforts. Key indicators will be reported for the overall population and by Actions by Federal agencies and partners should build on and subgroups as data are available. Indicators and 10-year targets complement existing strategies, plans, and guidelines to improve are drawn from existing measurement efforts, especially Healthy health. Key documents that provide a more detailed set of People 2020. Detailed information about the key indicators recommendations or offer tools and resources are listed for can be found in Appendix 2. In some cases, data that can help each Strategic Direction and Priority (Appendix 6). In addition, describe the health status of certain populations are limited (e.g., because Healthy People 2020 is a foundational resource for all data on sexual orientation and gender identity, disability status). of the Strategic Directions and Priorities, relevant objectives are As data sources and metrics are developed or enhanced, National provided for each of the Strategy’s recommendations (Appendix Prevention Strategy’s key indicators and targets will be updated. 5). The Strategic Directions and Priorities also include include project highlights that show how communities have advanced prevention. These are provided for illustrative purposes to help * Examples do not indicate an official review or endorsement of any program or initiative. Programs must always be administered in accordance with applicable others consider ways in which they too can take action.* state and Federal laws. 12
- 13. National Prevention Strategy Leading Causes of Death Number of Deaths, 2007 Baseline (deaths per 10-Year Target Annually 100,000 population) Cancer 562,875 (23%) 178.4 160.6 Coronary Heart Disease 406,351 (17%) 126.0 100.8 Stroke 135,952 (6%) 42.2 33.8 Chronic Lower Respiratory Disease 127,924 (5%) 40.8 35.1 Unintentional Injury 123,706 (5%) 40.0 36.0 Note: The leading cause of death is diseases of the heart (2007 baseline: 616,067 deaths, 190.9 deaths per 100,000 population); however, coronary heart disease deaths will be tracked because they account for the majority (66%) of deaths from disease of the heart, are the most amenable to prevention, and have an available 10-year target established for Healthy People 2020. 13
- 14. Strategic Directions Healthy and Safe Community Environments Health and wellness are influenced by the places in which people live, learn, work, and play. Communities, including homes, schools, public spaces, and work sites, can be transformed to support well-being and make healthy choices easy and affordable. Healthy and safe community environments include those with clean air and water, affordable and secure housing, sustainable and economically vital neighborhoods (e.g., efficient transportation, good schools), and supportive structures (e.g., violence free places to be active, access to affordable healthy foods, streetscapes designed to prevent injury).8 Healthy and safe community environments are able to detect and respond to both acute (emergency) and chronic (ongoing) threats to health.9 Recommendations: What can be done? KEY FACTS Making places healthier requires capacity for planning, delivering, and evaluating • A variety of health-related hazards prevention efforts. A prevention-oriented society can be supported by integrating health are disproportionately found in and health equity criteria into community planning and decision making whenever low-income housing, including appropriate; maintaining a skilled, cross-trained, and diverse prevention workforce; excess moisture or mold, allergens, strengthening the capacity of state, tribal, local, and territorial health departments; poor indoor air quality, structural implementing effective policies and programs that promote health and safety; and deficiencies, and lead contamination.10 enhancing cross-sector data sharing and collaboration.16 • Exposures to environmental and occupational hazards before and 1 Improve quality of air, land, and water. Safe air, land, and water during pregnancy can increase risk are fundamental to a healthy community environment.17 Implementing and enforcing of subsequent health problems for environmental standards and regulations, monitoring pollution levels and human exposures, infants and children, such as birth and considering the risks of pollution in decision making can all improve health and the defects, developmental disabilities, quality of the environment.18 For example, air quality standards, improved fuel efficiency and and childhood cancer.11 use of cleaner fuels, and transportation choices that reduce dependency on automobiles all • Children may be more vulnerable to improve air quality and health.19 Safe drinking water is assured through routine monitoring, environmental exposures than adults detection, and notification of water-related risks to prevent chemical and biological because their bodily systems are still contamination.20 Monitoring and research to understand the extent of people’s exposure to developing and their behavior can environmental hazards, the extent of disparities in exposures and risks from environmental expose them more to chemicals and hazards and the impact of these exposures on health, and identifying how to reduce organisms.12 exposures, especially among vulnerable populations, will inform future efforts.18 • Nearly one in 10 (approximately 7 million) children aged 17 and under 2 Design and promote affordable, accessible, safe, and have asthma. Black children are more healthy housing. Living environments, including housing and institutional settings, likely to have asthma (17 percent) can support health.21 Quality housing is associated with positive physical and mental than Hispanic children (8 percent) well-being.22 How homes are designed, constructed, and maintained, their physical or non-Hispanic white children (8 characteristics, and the presence or absence of safety devices have many effects on injury, percent). Environmental factors (e.g., illness, and mental health.23 Housing free of hazards, such as secondhand smoke, pests, pests, mold and pollen, tobacco or carbon monoxide, allergens, lead, and toxic chemicals, helps prevent disease and other wood smoke, indoor and outdoor air health problems.24 Housing that meets universal design standards allows people, including pollution) exacerbate asthma.13 those with disabilities and older adults, to live safely in their homes.25 • Work-related factors, including Inadequate Housing* Rates Are Highest Among Blacks, Hispanics, occupational exposures to chemicals, and American Indian/Alaska Natives physical overexertion or inactivity, Percentage of Individuals Living 10 excessive heat or cold, noise, and 9.0% psychosocial factors (e.g., stress, 8 in Inadequate Housing 7.8% 7.5% job strain) can create or worsen a 6 variety of health problems including 4 4.6% 4.1% cancer, chronic obstructive pulmonary 2 disease, asthma, and heart disease.14 • Perceptions of safety and physical 0 White, Hispanic Black, Asian/Pacific American Indian/ surroundings influence individuals’ non-Hispanic non-Hispanic Islander Alaskan Native *Inadequate housing: moderate or severe deficiencies in plumbing, heating, electricity, or upkeep, or a combination decisions to walk in their of these. This data represents individuals, not households. neighborhoods.15 Source: American Housing Survey, U.S. Census Bureau, 2009 14
- 15. National Prevention Strategy 3 Strengthen state, tribal, local, and and optimize investments Green Technologies territorial public health departments to can help foster livable, Using green technologies provide essential services. Public health departments affordable, and healthy communities.33 Community (e.g., green buildings, provide the cornerstone of our nation’s public health capacity measures that include health renewable energy, energy and are critical in identifying and responding to the needs of their can be used to benchmark efficiency, and green communities.26 Strengthening surveillance and laboratory capacity existing conditions, set chemistry) can help reduce allows health departments to identify communities at greatest risk; performance targets, track use of energy, water, and measure the impact of policy, systems, and environmental changes; and communicate progress other resources as well as detect, control, and prevent infectious diseases; and respond to toward achieving community decrease pollution. Green outbreaks and emergencies.27 Systems to support quality—such outcomes, and increase technologies not only as quality improvement and management systems—promote accountability.34 Integrating improve the environment accountability and performance improvements.28 diverse measures (e.g., but can also make people healthier. For example, 4 Integrate health criteria into decision health, transportation, improving air quality making, where appropriate, across multiple economic, housing, public reduces respiratory and sectors. Assessments and audits (e.g., health impact safety, education, land use, air quality) provides a more cardiovascular diseases such assessments) can be used to help decision makers evaluate comprehensive assessment of as asthma and heart attacks. project or policy choices to increase positive health outcomes and minimize adverse health outcomes and health inequities. community well-being.35 Understanding all risks and impacts of municipal planning or investment decisions, including those that can affect health, 6 Expand and increase access to information technology will help ensure that land use and transportation investments and integrated data systems to promote cross-sector are aligned with positive and equitable health outcomes.29 information exchange. Timely, reliable, and coordinated data, Communities can be designed to increase physical activity, information, and communication increase capacity to plan and decrease motor vehicle and pedestrian injuries and fatalities, implement prevention strategies as well as detect and respond improve air quality, and reduce greenhouse gas emissions.30 to threats to the public’s health.36 Access to high quality, timely Locating schools, housing, nursing homes, and other key information is dependent on interoperable data systems, including community resources away from high-pollution areas such as mechanisms for data sharing and standards for data collection, highways and factories can reduce hospitalizations due to heart privacy protection, and analysis.37 Linked data systems and metrics attacks and respiratory disease.31 Providing affordable, accessible from a wide range of sectors and partners (e.g., health care, public transportation options and safe and navigable streets helps health, emergency response, environmental, justice, transportation, people, especially older adults, people with disabilities, and labor, worker safety, and housing) can support decision making.38 those with low incomes, to live safely in their communities, reach Integrating key data systems can also help streamline eligibility essential destinations (e.g., grocery stores, schools, employment, requirements and expedite enrollment to facilitate access to health health care, and public health services), and lead more rewarding and social services.39 and productive lives.32 7 Identify and implement strategies that 5 Enhance cross-sector collaboration are proven to work and conduct research in community planning and design to where evidence is lacking. Community-level promote health and safety. Coordinating efforts implementation of prevention policies and programs that have across sectors and governmental jurisdictions to prioritize needs a strong evidence base and are cost-effective can help ensure Key Indicators Current 10-Year Target Number of days the Air Quality Index (AQI) exceeds 100 11 days 10 days Amount of toxic pollutants released into the environment 1,950,000 tons 1,750,000 tons Proportion of state public health agencies that can convene, within 60 minutes of notification, a team of trained staff who can make decisions about appropriate response and interaction 84.0% 98.0% with partners Proportion of children aged 5 to 17 years with asthma who missed school days in the past 12 months 58.7% 48.7% 15
- 16. Strategic Directions Healthy and Safe Community Environments that efforts are effective and efficient.40 Additionally, promising, chronic diseases, promote innovative approaches to improve health and wellness, especially safety, and eliminate health Increasing the Ability of those drawn from practice-based experience, are important to disparities. Health Professionals to test.41 Cross-sector collaborative research (e.g., transportation, • Use housing development Identify, Prevent, and education, labor, environment, criminal justice, housing, health) subsidies to promote Reduce Environmental can identify opportunities for policy and program alignment and mixed-income Health Threats be used to guide decision making.42 neighborhoods and Clinicians can provide access to safe and healthy information and counseling 8 Maintain a skilled, cross-trained, and housing. on how to prevent, treat, diverse prevention workforce. Recruiting and • Support state, tribal, local, and manage environmental- retaining a skilled and diverse prevention workforce strengthens and territorial partners to related exposures. Through our capacity to promote health and respond to emergencies.43 To enhance epidemiology and Pediatric Environmental be effective, the prevention workforce must include health care laboratory capacity, health Health Specialty Units, providers, public health workers, community health workers, and information technology, Federal agencies are also professionals outside of traditional health-related fields (e.g., and performance partnering with the health transportation, education, housing, labor). The workforce must improvement. care community to help have the tools and skills needed to promote health in the 21st • Support state, tribal, local, clinicians assist parents in century, including health information technology, informatics, and territorial partners in addressing environmental health literacy, and policy analysis and implementation.44 Cross- strategic health security health concerns (e.g., indoor training and recruiting diverse professionals (e.g., economists, planning efforts for air pollutants, lead, mercury, scientists, psychologists, criminologists, urban planners, architects, pandemics, biological and and pesticides). engineers, home inspectors) can enhance delivery of prevention chemical attacks, incidents and health promotion strategies.45 affecting food and agriculture, natural disasters, and other catastrophic events. • Support effective public safety measures, such as community- Actions based anti-crime and anti-gang initiatives to facilitate physical The Federal Government will activity and prevent injury and violence. • Coordinate investments in transportation, housing, environmental protection, and community infrastructure to promote sustainable and healthy communities. Partners Can • Enhance capacity of state, tribal, local, and territorial State, Tribal, Local, and Territorial Governments can governments to create healthy, livable and sustainable • Facilitate collaboration among diverse sectors (e.g., communities (e.g., increase access to healthy food and planning, housing, transportation, energy, education, opportunities for physical activity, revitalize brownfields, environmental regulation, agriculture, business associations, enhance alternative transportation options, and develop green labor organizations, health and public health) when making facilities and buildings). decisions likely to have a significant effect on health. • Support standards to reduce pollution and environmental • Include health criteria as a component of decision making exposure to ensure that all communities are protected from (e.g., policy making, land use and transportation planning). environmental and health hazards. • Conduct comprehensive community health needs assessments • Support healthy housing while addressing unsafe housing and develop state and community health improvement plans. conditions and health-related hazards, including injury hazards, • Promote the use of interoperable systems to support data- asthma triggers, and lead-based paint hazards. driven prevention decisions and implement evidence-based • Increase availability and use of prevention research to identify prevention policies and programs, such as those listed in the effective environmental, policy, and systems that reduce Guide to Community Preventive Services. PROJECT HIGHLIGHT: Partnership for Sustainable Communities The Partnership for Sustainable Communities helps communities become economically strong and environmentally sustainable. Guided by six livability principles, the Environmental Protection Agency and Departments of Housing and Urban Development and Transportation are coordinating investments and aligning policies to give Americans more housing choices, make transportation systems more efficient and reliable, and support vibrant and healthy neighborhoods that attract businesses. 16
- 17. National Prevention Strategy PROJECT HIGHLIGHT: Neighborhood Revitalization Initiative The Neighborhood Revitalization Initiative (led by the White House Domestic Policy Council, White House Office of Urban Affairs, and the Departments of Housing and Urban Development, Education, Justice, Health and Human Services, and Treasury) supports the transformation of distressed neighborhoods into neighborhoods of opportunity – places that provide the right combination of circumstances, resources, and environments that both children and adults need to thrive. Key elements include high-quality schools and educational programs; safe and affordable housing; thriving commercial establishments; varied cultural amenities; and parks and other recreational spaces. • Strengthen and enforce housing and sanitary code related to community planning and development (e.g., requirements and ensure rapid remediation or alternative urban planning, architecture and design, transportation, housing options. civil engineering, agriculture) and encourage innovation in • Participate in national voluntary accreditation of health designing livable, sustainable communities. departments. • Implement policies and practices that promote healthy and safe environments (e.g., improving indoor air quality; Businesses and Employers can addressing mold problems; reducing exposure to pesticides • Ensure that homes and workplaces are healthy, including and lead; ensuring that drinking water sources are free from eliminating safety hazards (e.g., trip hazards, unsafe stairs), bacteria and other toxins; implementing and enforcing tobacco ensuring that buildings are free of water intrusion, indoor free policies). environmental pollutants (e.g., radon, mold, tobacco smoke), and pests, and performing regular maintenance of heating and Community, Non-Profit, and Faith-Based cooling systems. Organizations can • Adopt practices to increase physical activity and reduce • Convene diverse partners and promote strong cross-sector pollution (e.g., workplace flexibility, rideshare and vanpool participation in planning, implementing, and evaluating programs, park-and-ride incentives, travel demand community health efforts. management initiatives, and telecommuting options). • Implement processes to ensure that people are actively • Identify and implement green building siting, design, engaged in decisions that affect health. construction, operations, and maintenance solutions that over time will improve the environment and health. Individuals and Families can • Adhere to best practices to promote safety and health, • Use alternative transportation (e.g., biking, walking, public including participatory approaches to hazard identification and transportation, car and vanpooling). remediation as well as supervisory and worker training. • Conduct home assessments and modifications (e.g., installing smoke and carbon monoxide detectors, testing for lead, Health Care Systems, Insurers, and Clinicians can checking for mold and radon). • Partner with state, tribal, local, and territorial governments, • Purchase energy-efficient products, support local vendors, business leaders, and community-based organizations to and recycle. conduct comprehensive community health needs assessments and develop community health improvement plans. • Support integration of prevention and public health skills into health care professional training and cross train health care practitioners to implement prevention strategies. KEY DOCUMENTS • Increase the use of certified electronic health records to identify • Environmental Protection Agency’s Report on the populations at risk and develop policies and programs. Environment • America’s Children: Key National Indicators of Well-Being Early Learning Centers, Schools, Colleges, and • The Surgeon General’s Call to Action to Promote Healthy Universities can Homes • Integrate appropriate core public health competencies • Recommendations for Improving Health through into relevant curricula (e.g., nursing, medicine, dentistry, Transportation Policy allied health, pharmacy, social work, education) and train • Partnership for Sustainable Communities: A Year of Progress professionals to collaborate across sectors to promote health for American Communities and wellness. • Priority Areas for Improvement of Quality in Public Health • Include training on assessing health impact within fields 17
- 18. Strategic Directions Clinical and Community Preventive Services Evidence-based preventive services are effective in reducing death and disability, and are cost-effective or even cost-saving. Preventive services consist of screening tests, counseling, immunizations or medications used to prevent disease, detect health problems early, or provide people with the information they need to make good decisions about their health. While preventive services are traditionally delivered in clinical settings, some can be delivered within communities, work sites, schools, residential treatment centers, or homes. Clinical preventive services can be supported and reinforced by community-based prevention, policies, and programs. Community programs can also play a role in promoting the use of clinical preventive service and assisting patients in overcoming barriers (e.g., transportation, child care, patient navigation issues). Recommendations: What Can Be Done? KEY FACTS Increasing use of preventive services depends on the health care • Less than half of older adults are up-to-date on a core set system’s ability to deliver appropriate preventive services as well of clinical preventive services (e.g., cancer screening and as people’s understanding of the benefits of preventive care and immunizations).46 their motivation and ability to access services. The Affordable • On average, 42,000 deaths per year are prevented among Care Act expands access to clinical preventive services by helping children who receive recommended childhood vaccines.47 more people obtain health coverage and removing cost-sharing • Brief clinician counseling is effective in helping people quit for clinical preventive services ranked “A” or “B” by the U.S. using tobacco; however, less than 20 percent of current Clinical Preventive Services Task Force. Many more people will tobacco users report receiving tobacco cessation counseling receive needed preventive care if logistical, financial, cultural, and during their most recent office visit with a clinician.48 health literacy barriers to care are removed and if information • Less than half of Americans with hypertension have and clinical supports are available to clinicians. Furthermore, adequately controlled blood pressure and only a third with quality of care will be improved if clinical, community, and high cholesterol have it adequately controlled.49 Improving complementary services are integrated and mutually reinforcing. control is one of the most effective ways to prevent heart disease and stroke.50 1 Support the National Quality Strategy’s • Colorectal cancer is the second leading cause of cancer- focus on improving cardiovascular health. related death in the United States.51 Some estimates suggest The National Quality Strategy prioritizes interventions to prevent that if screenings were implemented at recommended levels, cardiovascular disease, which could save tens of thousands of lives more than 18,000 lives could be saved each year.52 each year.57 The highest-value services that are both evidence- • Each year, asthma costs the U.S. about $3,300 per person based and cost-effective include Aspirin, Blood pressure control, (with asthma) in medical expenses, missed school and work Cholesterol reduction, and Smoking cessation (the “ABCS”).58 days, and early deaths. Some of the 12 million annual Activities that can improve heart health include reducing asthma attacks can be prevented through home visitation uncontrolled blood pressure and cholesterol, decreasing sodium and programs that assess and modify homes to reduce exposure saturated and trans fat intake, eliminating smoking and exposure to to asthma triggers and educate individuals on how to secondhand smoke, increasing aspirin use to prevent and reduce the improve asthma self-management.53 severity of heart attacks and strokes, and lifestyle interventions to • Diabetes is the leading cause of heart disease and stroke, modify risk factors such as obesity and physical inactivity.59 blindness, kidney failure, and lower-extremity amputation. Blood pressure control reduces the risk of cardiovascular The Majority of Americans with High Blood Pressure disease (heart disease and stroke) among people with or High Cholesterol Do Not Have It Controlled diabetes by 33 to 50 percent and the risk of microvascular 80 disease (eye, kidney and nerve disease) by approximately 33 U.S. Adults – in millions 70 71 percent.54 Community programs that teach people how to 60 68 manage their diabetes can help prevent short- and long-term 50 40 48 health conditions, enhance individuals’ quality of life, and 30 31 34 contain health care costs.55 20 23 • More than 80 million people in the U.S. do not have access to 10 0 fluoridated water. Water fluoridation reduces tooth decay by High Blood Pressure High Cholesterol* 25 percent in children and adults, and every dollar spent on Total Diagnosed Treated Controlled fluoridation saves more than $40 in dental treatment costs.56 *Indicates low-density lipoprotein cholesterol Source: National Health and Nutrition Examination Survey, 2005–2008 18
- 19. National Prevention Strategy 2 Use payment and reimbursement reporting systems that make health and clinical information mechanisms to encourage delivery of available empowers people to make more informed decisions and clinical preventive services. The Affordable Care better manage their care.62 Electronic health records and other Act ensures that new private health plans and Medicare cover health information technology can enhance the quality and value certain preventive services without cost sharing, and provides of health care, but only if there are appropriate protections in incentives for States to do so through Medicaid. Making place to keep health information private and secure. Patients and preventive services free at the point of care is critical to increasing providers must feel confident that laws, policies, and processes their use, but it is not sufficient.57 Delivery of clinical preventive are in place to keep their health information private and secure, services increases when clinicians have billing systems in place to and that they will be enforced when violations occur. facilitate appropriate reimbursement for providing these services. Furthermore, payment systems can incentivize quality and value 4 Support implementation of community- of care (e.g., by increasing reimbursements for improving patient based preventive services and enhance outcomes). Reimbursement mechanisms focused on proven linkages with clinical care. Clinical and community interventions (e.g., those that support team-based care; use prevention efforts should be mutually reinforcing—people nonphysician clinicians such as nurse practitioners, physician should receive appropriate preventive care in clinical settings assistants, pharmacists, and community health workers; and (e.g., a clinician providing tobacco cessation counseling and implement bundled payment systems) and measurable treatment medication) and also be supported by community-based outcomes can increase delivery of preventive services.60 In resources (e.g., tobacco cessation quitlines).63 Clinicians can addition, preventive services and medications can be made more refer patients to community-based prevention resources such as affordable through approaches such as health benefit design or programs for blood pressure and cholesterol control or home- facilitating entry of generic drugs into the market.61 based interventions to control asthma triggers.64 Additionally, some preventive services can be delivered effectively outside of 3 Expand use of interoperable health traditional medical settings (e.g., measuring blood pressure or information technology. Patients, clinicians, and adjusting medication regimens through community pharmacies).65 health care systems can use health information technology to Work site and school clinics can also provide convenient points of improve delivery of clinical preventive services, improve quality care for traditionally underserved populations.66 of care, and reduce health care costs.62 Certified electronic health records with decision support can prompt clinicians to implement 5 Reduce barriers to accessing clinical and evidence-based practices tailored to individual health needs.60 community preventive services, especially Clinicians or health care systems can receive feedback on their among populations at greatest risk. When people rate of delivery of clinical preventive services and be recognized are motivated to seek care and have a primary care clinician, they or rewarded for their performance. Monitoring and public are more likely to access health services.67 Locating clinical services Key Indicators Current 10-Year Target Proportion of medical practices that use electronic health records 25.0% 27.5% Proportion of adults aged 18 years and older with hypertension whose 43.7% 61.2% blood pressure is under control Proportion of adults aged 20 years and older with high low-density 33.2% 36.5% lipoprotein (LDL) cholesterol whose LDL is at or below recommended levels Proportion of adults aged 50 to 75 years who receive colorectal cancer screening 54.2% 70.5% based on the most recent guidelines 6 – 23 months: 23.0% 80.0% 2 – 4 years: 40.0% 80.0% Proportion of children and adults who are vaccinated annually against 5 – 12 years: 26.0% 80.0% seasonal influenza 13 – 17 years: 10.0% 80.0% 18 – 64 years: 24.9% 80.0% 65 years and older: 67.0% 90.0% Patients, clinicians, and health care systems can use electronic health records to improve delivery of clinical preventive services and improve the quality of preventive care. This key indicator is being reassessed in light of recent ACIP recommendations and data sources. 19
- 20. Strategic Directions Clinical and Community Preventive Services conveniently near homes or workplaces, as well as logistical factors (especially those in underserved populations) about coverage (e.g., adequate transportation, time off for workers, child care), improvements and elimination of cost-sharing for clinical can all help facilitate access.68 Community health workers and peer preventive services as set forth in the Affordable Care Act. support can also facilitate access to and use of preventive services, • Encourage adoption of certified electronic health record especially among vulnerable populations.69 technology that meets Meaningful Use criteria, particularly those that use clinical decision supports and registry 6 Enhance coordination and integration functionality, send reminders to patients for preventive and of clinical, behavioral, and complementary follow-up care, provide patients with timely access to their health strategies. Integrated health care describes health information (e.g., lab results, discharge instructions), a coordinated system in which health care professionals are identify resources available to patients, and incorporate privacy educated about each other’s work and collaborate with one and security functions (e.g., encrypting health information to another and with their patients to achieve optimal patient well- keep it secure, generating audit logs to record actions). being.70 Implementing effective care coordination models (e.g., • Improve use of patient-centered medical homes and medical homes, community health teams, integrated workplace community health teams, which are supported by the health protection and health promotion programs) can result Affordable Care Act. in delivery of better quality care and lower costs.71 Gaps and • Promote and expand research efforts to identify high-priority duplication in patient care, especially among those with multiple clinical and community preventive services and test innovative chronic conditions, can be reduced or eliminated through strategies to support delivery of these services. technologies (e.g., electronic health records, e-prescribing, • Develop new and improved vaccines, enhance understanding telemedicine).72 Evidence-based complementary and alternative of the safety of vaccines and vaccination practices, support medicine focuses on individualizing treatments, treating the whole informed vaccine decision-making, and improve access to and person, promoting self-care and self-healing, and recognizing better use of recommended vaccines. the spiritual nature of each individual, according to individual • Research complementary and alternative medicine strategies to preferences.73 Complementary and alternative therapies for determine effectiveness and how they can be better integrated back and neck pain (e.g., acupuncture, massage, and spinal into clinical preventive care. manipulation) can reduce pain and disability.74 Partners Can Actions State, Tribal, Local, and Territorial Governments can The Federal Government will • Increase delivery of clinical preventive services, including • Support delivery of clinical preventive services in various ABCS, by Medicaid and Children’s Health Insurance Program health care and out-of-home care settings, including Federally (CHIP) providers. Qualified Health Centers; Bureau of Prisons, Department of • Foster collaboration among community-based organizations, Defense, and Veterans Affairs facilities; and among Medicare the education and faith-based sectors, businesses, and providers. clinicians to identify underserved groups and implement • Improve monitoring capacity for quality and performance of programs to improve access to preventive services. recommended clinical preventive services. • Create interoperable systems to exchange clinical, public health • Identify, pilot, and support strategies to reduce cardiovascular and community data, streamline eligibility requirements, and disease, including improving screening and treatment for high expedite enrollment processes to facilitate access to clinical blood pressure and cholesterol. preventive services and other social services. • Encourage older adults to seek a free annual Medicare wellness • Expand the use of community health workers and home visit, a new benefit provided by the Affordable Care Act. visiting programs. • Educate clinicians, Federal employees, and the public PROJECT HIGHLIGHT: Diabetes Prevention and Control Alliance A partnership between UnitedHealth Group, the YMCA of the USA, and retail pharmacies, the Diabetes Prevention and Control Alliance helps to enhance linkages between clinical and community-based preventive services through innovative programming. The Diabetes Prevention Program helps people with prediabetes eat healthier, increase physical activity, and learn about other health-promoting behavior modifications. The Diabetes Control Program links people with diabetes to local pharmacists who are trained to help them manage their condition and follow their physicians’ treatment plans.* * Employment-based group health plans should always check to ensure that any benefits provided by the plan comply with applicable state and Federal laws. 20
