Organ Transplantation: A Historical Overview
- 1. Organ Transplantation Professor Richard Frank, MSN, RN
- 2. A Few Key Historical Facts: • 1954: First successful kidney transplant performed • 1968: Uniform Anatomical Gift act signed • 1968: First organ procurement organization (OPO) established, New England Organ Bank (based in Boston) • 1983: FDA approved cyclosporine anti-rejection medication • 1984: National Organ Transplant Act operated by UNOS • 1998: Plasmapheresis introduced; enabled kidney transplants in patients whose blood group/antibodies incompatible with donor • 1998: First successful hand transplant performed in France • 2011: First successful full face transplant performed in the US (Boston, MA)
- 3. 1968: Uniform Anatomical Gift • Establishes uniform organ donor card as a legal document. • Next of kin can donate without the presence of a donor card. • Website
- 4. 1984: National Organ Transplant Act • National Organ Transplant Act (NOTA) maintained by the United Network for Organ Sharing (UNOS) • Authorizes financial support for Organ Procurement Organizations (OPOs); prohibits buying or selling of organs in the United States. • Website
- 5. 1986: Required Request Law • Requires hospitals to develop policies to identify patients as potential donors • Requires hospitals to approach families regarding organ donation
- 6. 1998: National Conditions of Participation Legislation • Requires hospitals to refer all deaths and imminent deaths to the local procurement organization.
- 7. LET’S REVIEW … Uniform Anatomical Gift: _________________________________________________________ _________________________________________________________ National Organ Transplant Act: ________________________________________________________ ________________________________________________________ Required Request Law: ________________________________________________________ ________________________________________________________ National Conditions of Participation Legislation: ________________________________________________________ ________________________________________________________
- 8. Organ & Tissue Transplantation • Cornea • Kidneys • Skin • Bone marrow • Heart and heart valves • Intestine • Bone • Lung • Liver • Pancreas
- 9. Who Can Donate? • Direct Donation • Non-Direct Donation • Living Donor • Cadaver Donor
- 10. Determining Brain Death & the Uniform Brain Death Act • Irreversible coma • Unresponsive to all stimuli • Absence of spontaneous muscle activity • Irreversible cessation of circulatory and respiratory function • Isoelectric electroencephalogram (EEG) for 30 minutes
- 11. The Different Types of Organ Donors: • Types of Living Donor Transplants • Kidney (entire organ) • Liver (segment) • Lung (lobe) • Intestine (portion) • Pancreas (portion) • After brain death • Kidney • Heart • Liver • Lungs • Pancreas • Intestine • Heart valves • Connective tissue • Cadaver • After natural death • Cornea • Bone • Skin • Blood vessels Living -Relative -Stranger Cadaver
- 12. Types of Transplants • Autograft • Allograft • Isograft • Xenograft
- 13. LET’S REVIEW … Who Can Donate? _______________________________________________________ ________________________________________________________ How is Brain Death Determined? ________________________________________________________ ________________________________________________________ Uniform Determination of Death Act: ________________________________________________________ ________________________________________________________ What are the Different Type of Organ Donors? ________________________________________________________ ________________________________________________________ What are the Different Types of Transplants? ________________________________________________________ ________________________________________________________
- 14. Liver Transplant • End-stage liver disease • Chronic viral hepatitis • Live and cadaver donors • Post-op complications • Rejection • Infection • Nursing Care • Neuro assessment • Hemorrhage • Respiratory assessment • Urinary output • Labs • Vital signs • Assess for s/s of infection and rejection
- 15. Heart Transplant •End-stage heart failure • Patient dependant on inotropes • Refractory cardiogenic shock •Cardiomyopathy •Inoperable CAD
- 16. Lung Transplant • End-stage lung disease • 4 types of surgery • Single lung • Bilateral lung • Heart-lung • Lobe transplant • Post-op care • Ventillatory support • Hemodynamic monitoring • Immunosuppressive therapy • Monitor for s/s of infection and rejection • Website
- 17. LET’S REVIEW … LIVER Transplant: _______________________________________________________ _______________________________________________________ _______________________________________________________ LUNG Transplant: _______________________________________________________ _______________________________________________________ _______________________________________________________ HEART Transplant: ________________________________________________________ ________________________________________________________ ________________________________________________________
- 18. How are organs allocated? •ABO blood type •Medical urgency •Time on the waiting list •Geographic location
- 19. United Network for Organ Sharing (UNOS) • Coordinates the organ transplant system in the United States • Increases public awareness of the critical need for donated organs and tissues • Maintains the national organ transplant waiting list • Coordinates the matching and distribution of donated organs • Collects and reports data on transplant recipients, donors and outcomes
- 20. Organ Procurement Organizations (OPOs) •Responsible for recovering the organ and keeping it viable until it is transplanted, and transporting the organ to the recipient •New England Organ Bank: oldest OPO in the US • Covers the 6 New England states and Bermuda • OPO procurement coordinator will take over the care of the donor until surgery
- 21. Organ Donor Waiting list: Data source: http://optn.transplant.hrsa.gov/
- 22. Prioritizing Patients for Transplantation • Each organ type has its own individual distribution policy • Patients who are close biological matches with a particular donor offer are given priority • Patients whose medical status is most urgent receive priority • Organs are offered locally first • Children are often offered priority • Wait time is used to break ties between patients who are similar
- 23. UNOS Regional Map Region 1 - Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island Region 2 - Delaware, District of Columbia, Maryland, New Jersey, Pennsylvania, Northern Virginia, West Virginia Region 3 - Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Puerto Rico Region 4 - Oklahoma, Texas Region 5 - Arizona, California, Nevada, New Mexico, Utah Region 6 - Alaska, Hawaii, Idaho, Montana, Oregon, Washington Region 7 - Illinois, Minnesota, North Dakota, South Dakota, Wisconsin Region 8 - Colorado, Iowa, Kansas, Missouri, Nebraska, Wyoming Region 9 - New York, Vermont Region 10 - Indiana, Michigan, Ohio Region 11 - Kentucky, North Carolina, South Carolina, Tennessee, Virginia
- 24. LET’S REVIEW … ORGAN ALLOCATION: ________________________________________________________ ________________________________________________________ ________________________________________________________ ONUS: ________________________________________________________ ________________________________________________________ ORGAN PRIORITIZATION FOR TRANSPLANTATION: ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ UNOS REGIONS: ________________________________________________________ ________________________________________________________
- 25. Organ offer process •Deceased organ donor is identified •UNOS notifies transplant team of the first person on the match list •Potential recipient must be available 24 hours a day •Given one hour to accept or turn down the organ • Evaluated for presence of infection • Admit to hospital for pre-op
- 28. Human leukocyte antigen typing (HLA) • HLA antigens are detected on the surface of White Blood Cells. • Regulates how the body recognizes and rejects foreign tissue. • There are 5 loci with 2 antigens at each locus (total of 6 antigens) • A, B, C, D and DR • The goal is to match as many antigens as possible • Certain organs and tissue transplants require a closer match than other organs
- 29. Human leukocyte antigen (HLA) type
- 30. LET’S REVIEW … ORGAN OFFERING:________________________________________ ________________________________________________________ ________________________________________________________ UNOS & OPOs: ___________________________________________ ________________________________________________________ ________________________________________________________ PRIORITIZATION: _________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________
- 31. Transplant Rejection Transplant rejection • Hyperacute • Occurs minutes to hours after transplantation • No treatment (organ must be removed) • Acute • Occurs days (one week) to months after transplantation • T- cytotoxic lymphocytes attack the transplanted organ • Chronic • Occurs over months to years • Most common in lung transplants Some Common Signs & Symptoms • Pain at the site of the transplant • Feeling ill • Flu-like symptoms • Fever • Weight change • Swelling • Decreased urine output
- 32. Immunosuppressive Therapy •Triple therapy (all PO/IV) • Cyclosporine • Prevent a cell-mediated attack (helper T-cells) against the organ • Corticosteriod: prednisone-methylprednisolone (Solu- Medrol) • Suppress inflammatory response • Cytotoxic drug: mycophenolate mefetil (CellCept) or cyclophosphamide (Cytoxan) • Suppress immune response by inhibiting proliferation of T and B cells •Monoclonal Antibodies: muromonab-CD3 • Used for preventing and treating acute rejection episodes •Polyclonal Antibodies: Atgam • Used as induction therapy or to treat acute rejection
- 33. Calcineurin inhibitor: Cyclosporine •Most effective immunosuppressant available •Prevents cell mediated attack against the new organ •Potentially nephrotoxic •Avoid grapefruit juice •Side effects • Nephrotoxicity • Increased risk of infection • Neurotoxicity (seizure activity, tremor) • Hepatotoxicity • Lymphoma • Hypertension • Gingiveal hyperplasia
- 34. Corticosteroids: Prednisone, Methylprednisolone, Solu-Medrol •Very effective in suppressing the inflammatory response but large doses are associated with adverse effects • Altered wound healing • Altered metabolism of fats, proteins, and carbohydrates • Increased blood glucose levels • Emotional disturbance • Osteoparosis • Change in fat distribution: cushingoid appearance • Moon face • Increased truncal fat • Buffalo hump
- 35. Cytotoxic Drug: mycophenolate (CellCept) •Suppresses T and B lymphocytes •Decreases the incidence of graft loss •Side effects •GI toxicity n/v/d •Neutropenia •Thrombocytopenia •Increased risk of infection •Increased risk of malignancy
- 36. Monoclonal Antibodies: muromonab- CD3, orthoclone OKT-3 •Used in preventing and treating acute rejection episodes •The antiantigen receptor antibody interferes with the function of the T-lymphocytes •Given IV push 7-14 days •All T-cells are affected with in minutes of administering the drug and the number of circulating T-cells decrease rapidly •Associated with terrible side effects
- 37. Polyclonal Antibody: Atgam •Used to as induction therapy •Side effects • Fever • Chills • Muscle and joint pain • Increased heart rate • Back pain • Shortness of breath • Hypotension • Rash • Increased risk of infection
- 38. Immunosuppressive Therapy: Side Effects •Nephrotoxicity •Increased risk of infection •Lymphoma •Hepatotoxicity •Neutropenia •Thrombocytopenia •Diarrhea/nausea/vomiting
- 39. LET’S REVIEW … REJECTION: ______________________________________________ ________________________________________________________ IMMUNOSUPPRESSIVE THERAPIES: ___________________________ ________________________________________________________ ________________________________________________________ ____ ____________________________________________________ ________________________________________________________ ________________________________________________________ IST SIDE EFFECTS: _________________________________________ ________________________________________________________ ________________________________________________________
- 40. Nursing Care of the Transplant Recipient •THE PATIENT •THE HOME •THE TRANSPLANT •INFECTION & REJECTION
- 41. Nursing Care of the Transplant Recipient •THE PATIENT: •Hand washing •Assess for infection •Restrict visitors who have minor upper respiratory infections
- 42. Nursing Care of the Transplant Recipient •THE HOME •Assess for graft vs host disease •Monitor labs •Reverse or protective isolation
- 43. Nursing Care of the Transplant DONOR •THE TRANSPLANT •Adequate nutrition •IV bags and tubing •Invasive lines and catheters
- 44. Nursing Care of the Transplant Recipient •INFECTION & REJECTION •Strict personal hygiene and mouth care •Assess for evidence of rejection •Strict medication regime
- 45. LET’S REVIEW … THE PATIENT: _____________________________________________ ________________________________________________________ ________________________________________________________ THE HOME:_______________________________________________ _________________________________________________________ THE TRANSPLANT: _________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ INFECTION & REJECTION: ___________________________________ ________________________________________________________
Editor's Notes
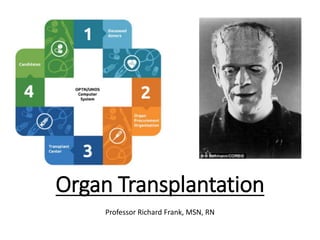
- Hello Class, Today we will be discussing Organ Transplantation. What is the history? Did Dr. Frankenstein do the very first head/brain transplant? Actually, World renowned neurosurgeon Dr. Sergio Canavero, thinks that such an operation is possible. He believes it would take 100 surgeons up to 36 hours and would cost approximately $17 million. You can read about it in the journal: Surgical Neurology International; 2013, Vol. 4, Suppl 6 - A Supplement to SNIHEAVEN: The head anastomosis venture Project outline for the first human head transplantation with spinal linkage (GEMINI) For now let’s look at other historically significant events.
- New England – particularly Boston - has figured prominently in the advancement of organ transplant in the United States. Your Med. Surg. Textbook doesn’t go into detail, but here is a timeline which shows key moments in history, as they relate to the evolution of organ transplantation.
- The Uniform Anatomical Gift Act (UAGA or the Act) was passed in the US in 1968 set a legislative precedent for the donation of fetal organs and tissues and has been in the background of many debates regarding abortion and fetal tissue research. It has since been revised in 1987 and in 2006. The Act sets a regulatory framework for the donation of organs, tissues, and other human body parts in the US. The UAGA helps regulate body donations to science, medicine, and education. The Act has been consulted in discussions about abortion, and fetal tissue transplants. Additionally, Body Worlds, the anatomy & physiology exhibit of real human bodies, preserved using plastination, has a body donation process to further the study of the body.
- It’s important to understand the history of how this country has gotten to where it is, related to the nation's critical organ donation shortage, organ matching and the placement process. In 1984 the U.S. Congress passed the National Organ Transplant Act* (NOTA). The act established the Organ Procurement and Transplantation Network (OPTN) to maintain a national registry for organ matching. The act also called for the network to be operated by a private, non-profit organization under federal contract. The current U.S. Code that has resulted from NOTA and its amendments can be found here: http://uscode.house.gov/search/criteria.shtml. Search for Title 42, Section 273.
- President Ronald Reagan signed the Required Request Law which mandates that hospital personnel discuss anatomical gifting with the relatives of a deceased patient. Required request law has been circulated as a means of increasing the rate of organ harvest and alleviating the critical shortage of transplantable organs. The Uniform Anatomical Gift Act mandates a required-request law. However, this Act is not in effect in all the states. Although the federal and many state governments have passed legislation to make such requests compulsory, the efficacy of this approach has not been demonstrated.
- Lastly, President Bill Clinton signed the National Conditions of Participation Law in order to provide an early assessment of hospitals’ and organ procurement organizations’ responses to Medicare conditions of participation designed to increase organ donation. This final rule establishes, for the first time, Medicare conditions of participation for heart, heart-lung, intestine, kidney, liver, lung, and pancreas transplant centers. Essentially, it tied federal funding (for hospitals who received Medicare money) to the organ transplant process. This rule sets forth clear expectations for safe, high quality transplant service delivery in Medicare-participating facilities.
- 18 people will die each day waiting for an organ 1 organ donor can save up to 8 lives. Organ transplantation has become an accepted medical treatment for end-stage organ failure. The facts prove it. But only you can help make it happen. Here are some important facts about donation: During your visit to organdonor.gov someone may have been added to the waiting list. It happens every 10 minutes. Each day, an average of 79 people receive organ transplants. However, an average of 18 people die each day waiting for transplants that can't take place because of the shortage of donated organs. People of every age give and receive organ donations. In 2012 a total of 28,051 people received organ transplants. Here’s the number of recipients by age group: 1 Year Old: 277 (252 deceased, 25 living donors) 1 - 5 Years: 520 (422 deceased, 98 living donors) 6 - 10 Years: 280 (220 deceased, 60 living donors) 11 - 17 Years: 695 (539 deceased, 156 living donors) 18 - 34 Years: 3,105 (2,010 deceased, 1,095 living donors) 35 - 49 Years: 6,386 (4,809 deceased, 1.577 living donors) 50 - 64 Years: 12,155 (10,096 deceased, 2,059 living donors) 65+ Years: 4,633 (3,839 deceased, 794 living donors)
- All people regardless of age should consider themselves potential organ and tissue donors. There are few absolute exclusions (such as HIV infection, active cancer, systemic infection) and no strict upper or lower age limits. Potential donors will be evaluated for suitability when the occasion arises. No one is too old or too young. Both newborns and senior citizens have been organ donors. The condition of your organs is more important than age. Someone 35 years old with a history of alcohol abuse may have a liver that is in worse condition than someone 60 years old who has never consumed alcohol. Doctors will examine your organs and determine whether they are suitable for donation if the situation arises. If you are under 18, you may need the permission of a parent or guardian to donate. >32% of donors last year were over the age of 50. > Your age doesn’t make you ineligible to sign up, nor do you have to be in perfect health. Your ability to donate is determined at the time of death. Organ and tissue transplants are needed by people in every corner of America. People of all ages, infants to grandparents, are on the national transplant waiting list. Two thirds of the individuals waiting for an organ transplant in 2012 were 50 years old or older. That year 2,250 deceased donors were between 50–64 years of age. Five hundred and seventy-four deceased donors were 65 or older. In 2012, 16,789 of the 28,053—or 59.8%—of the people transplanted were 50+. Medical Condition? You may still be able to donate your organs. Doctors will evaluate the condition of your organs when the time arises. The transplant team's decision will be based on a combination of factors such as your specific illness and your physical condition to determine which organs and tissues can be donated.
- Brain death occurs when the brain is totally and irreversibly non-functional. Brain death is caused by not enough blood supply of oxygen which causes the brain cells to die. In 1968 the first definition of brain death was published. It was based on neurological criteria developed by a Harvard Ad Hoc Committee. Uniform Brain Death Act (est. 1978) was created to clear up the legal ambiguity over the question of determining death. The Uniform Brain Death Act established that the "irreversible cessation of all functioning of the brain, including the brain stem" is death. The Uniform Determination of Death Act (UDDA) (est. 1980) added "irreversible cessation of circulatory and respiratory functions" as an alternative standard for determining death. The term "reasonable medical standards" has also been changed to "acceptable medical standards.“ It is concerned only with medical determination of biological death, and as such, complements existing and accepted definitions. The act does not specify an exact means of diagnosis. To do so would guarantee its obsolescence as technology advances. The purpose of the UDDA is a minimum one. It recognizes cardiorespiratory and brain death in accordance with the criteria the medical profession universally accepts. The act does not authorize euthanasia or "death with dignity," and does not enact any sort of living will. The current state of medical decision-making as it relates to death, termination of life, or other related issues remains unchanged. The UDDA simply attempts to relieve one relatively small problem in law and medicine, before it becomes a larger one.
- Living donors should be in good overall physical and mental health and older than 18 years of age. Some medical conditions could prevent you from being a living donor. Medical conditions that may prevent a living kidney donation may include uncontrolled high blood pressure, diabetes, cancer, HIV, hepatitis, acute infections, or a psychiatric condition requiring treatment. Since some donor health conditions could harm a transplant recipient, it is important that you share all information about your physical and mental health non–heart beating cadaveric donor a donor who has been pronounced dead according to the traditional criteria of lack of any pulse or detectable cardiac activity, but is not yet brain dead. There are two types: The controlled donor is a person in a vegetative state who has signed a consent form or otherwise stated his or her wishes before becoming ill. Based on the patient's stated wishes and at the request of the next-of-kin, cannulas are placed into blood vessels for postmortem cooling of organs and the person is removed from life support. Once death has been declared, the organs are rapidly perfused with cold preservative solution and surgically removed. The uncontrolled donor is a person declared dead because of catastrophic injury to the heart, such as a gunshot wound to the heart. Cannulas are placed into blood vessels after death and the organs are perfused and removed. This also requires consent of next-of-kin. Full body donation is one of the most compassionate alternatives to a funeral. Body donation is not the same as organ donation. Although organ donation is perhaps a better known alternative to a funeral, anatomical donation is an equally important gift to the future of humankind - and the cost of cremation is free. By donating your body to science, you're not only saving your family money, but are helping give surgeons a learning opportunity which may lead to a more efficient technique or a new life-saving surgical procedure. Full body donation makes cutting edge developments in the fields of cancer treatment, thoracic research and neurology studies possible. Anatomical donations allow research institutions to discover new ways to fight serious diseases and disorders such as cancer, Alzheimer's disease and multiple sclerosis.
- Autografts are the transplant of tissue to the same person. Sometimes this is done with surplus tissue, tissue that can regenerate, or tissues more desperately needed elsewhere (examples include skin grafts, vein extraction for CABG, etc.). Sometimes an autograft is done to remove the tissue and then treat it for the patient before returning it (examples include stem cell autograft and storing blood in advance of surgery). In a rotationplasty, a distal joint is used to replace a more proximal one; typically a foot or ankle joint is used to replace a knee joint. An allograft is a transplant of an organ or tissue between two genetically non-identical members of the same species. Most human tissue and organ transplants are allografts. Due to the genetic difference between the organ and the recipient, the recipient's immune system will identify the organ as foreign and attempt to destroy it, causing transplant rejection. An isograft is a subset of the allograft. Here and organs, or tissue, is transplanted from a donor to a genetically identical recipient (such as an identical twin). Isografts are differentiated from other types of transplants because while they are anatomically identical to allografts, they do not trigger an immune response. The xenograft is a transplant of organs or tissues from one species to another. An example is porcine (pig) heart valve transplant, which is quite common and successful. Another example is attempted piscine-primate (fish to non-human primate) transplant of islet (i.e. pancreatic or insular tissue) tissue. Xenotransplantion is a high risk type of transplant because of the increased risk of non-compatibility, rejection, and disease carried in the tissue.
- A liver transplant is the process of replacing a sick liver with a donated, healthy liver. Liver transplants require that the blood type and body size of the donor match the person receiving the transplant. Currently more than 6,000 liver transplants are performed each year in the United States. Liver transplant surgery usually takes between four and twelve hours. Most patients stay in the hospital for up to three weeks after surgery. Most donated livers come from people who recently died and had no liver injury. Non-living donors either have agreed to be organ donors or their families decide after they have passed away. When is a liver transplant needed? A liver transplant is needed when a person’s liver is failing and a doctor recommends he or she be evaluated for a transplant. Many diseases can cause liver failure. Cirrhosis (scarring of the liver) is the most common reason for liver transplants. Other common reasons for liver transplants are: Chronic hepatitis B and chronic hepatitis C, Bile duct diseases, Genetic diseases, Autoimmune liver diseases, Primary liver cancer, Alcoholic liver disease, and fatty liver disease How does a person become eligible for a liver transplant? After being referred by a doctor to a transplant center, the transplant team evaluates the person’s overall physical and mental health, plan to pay for transplant related medical expenses, and emotional support family and friends will provide. Based on these findings, the team decides if the person is eligible for a liver transplant. If the person is eligible, the center will add him or her to the national transplant waiting list. The waiting list is prioritized so the sickest people are at the top of the list. How long does a person wait for a liver transplant? The waiting time for a liver transplant is different for each person. The time a person spends on the waiting list depends on his or her blood type, body size, stage of liver disease, overall health, and the availability of a matching liver. In the United States, there are more people who need a liver transplant than there are donated livers. There are currently over 16,000 Americans on the waiting list for a liver transplant. What are the risks of a liver transplant? The most common risks associated with liver transplants are the body rejecting the liver and infections. Rejection occurs when the body’s immune system attacks an object it does not recognize. To prevent rejection, transplant patients are given medicines to weaken the immune system. Modern medications have made rejection less of a concern in liver transplant patients. Rejection medications may have side effects of increased blood pressure, headaches, diarrhea, and nausea. Also, because rejection medications weaken the immune system, it can be hard for liver transplant patients to fight infections.
- When is a heart transplant needed? The most common reason is that one or both ventricles have aren't functioning properly and severe heart failure is present. Ventricular failure can happen in many forms of congenital heart disease, but is more common in congenital defects with a single ventricle or if long-standing valve obstruction or leakage has led to irreversible heart failure. Patients who had the Fontan procedure (usually done at 2-4 years of age – a surgery that connects the inferior vena cava to the pulmonary artery, creating a channel through or just outside the heart to direct blood to the pulmonary artery), may need a heart transplant because the blood flow through the venous system is slow and the veins are congested, which can lead to swelling, fluid accumulation, and protein loss. How does a person become eligible for a heart transplant? We should look at the criteria that could reduce eligibility for transplant first: Older than 65, Severe irreversible pulmonary hypertension, Irreversible kidney or liver dysfunction not explained by underlying heart failure, Symptomatic peripheral, renal or cerebrovascular artery disease, severe chronic lung disease, such as Emphysema, asthma, or chronic bronchitis; Active systemic infection – which applies with all organ transplants, Insulin-dependent diabetes mellitus with evidence of damage to other organs, such as kidney, eye (retina), or nerves. How long is the wait? Unfortunately, the waiting times for heart transplants are long — often more than six months. Each patient on our waiting list returns for an outpatient visit to a transplant clinic every two to three months, or more frequently if necessary. Of course the wait is also dependent on the Region where the transplant candidate is registered. Many patients can wait at home. Organ transplant protocols guide candidates about how available they must be in the event a donor heart becomes available – often this is 1 hour within the operating facility. It is not uncommon for patients with advanced heart failure to be admitted to hospital for inotrope support, prior to a heart transplant. However, a prolonged hospital stay for inotrope therapy is expensive and is associated with substantial morbidity and lower quality of life. Risks are similar to those of liver transplant – organ rejection.
- A lung transplant may involve replacing one lung or both of them. In some situations, the lungs may be transplanted along with a donor heart. Living-donor lung transplants are rare. This procedure can replace a child's diseased lung with a section (lobe) of a lung taken from a healthy adult — usually a parent. Two living donors are needed if the procedure is used for an adult. Lung transplants aren't very common because of the small number of donor organs available. About 1,800 lung transplants were done in the United States in 2010. More donor lungs would mean a larger number of suitable lungs available for transplant. Most people who have lung transplants are between the ages of 18 and 65. Common indications for lung transplant include: Emphysema/COPD accounts for almost 1/3 of all lung transplants, other causes include Idiopathic pulmonary fibrosis , Cystic fibrosis , Alpha-1-antitrypsin deficiency (an inherited disorder which usually develops between ages 20 and 50 – see the website for more), Primary pulmonary hypertension, Sarcoidosis, Bronchiectasisi (a condition in which damage to the airways causes them to widen and become flabby and scarred), Obliterative bronchiolitis (non retransplant type). How does a person become eligible for a lung transplant? In general, you must be physiologically 60 years of age or less for bilateral lung transplantation and 65 years of age or less for single lung transplantation. This means that your physical condition must at least meet the typical condition of someone 60 years old or younger, or someone 65 years old or younger. Your chronological age is not a factor. You must have a poor prognosis, with an anticipated 18 to 24-month survival. You must have no other life-threatening systemic disease. You must have demonstrated absolute compliance with medications and medical recommendations, and have good rehabilitation potential. You must demonstrate emotional stability and must have a realistic understanding of the implications of organ transplantation. You must have a supportive social support system. How long is the wait for a Lung? Unfortunately the wait is similar to that for a heart transplant – and even longer because of the availability of matching donors.
- ABO-incompatible (ABOi) transplantation is a method of allocation in organ transplantation that permits more efficient use of available organs regardless of ABO blood type, which would otherwise be unavailable due to hyperacute rejection. Primarily in use in infants and young toddlers, research is ongoing to allow for increased use of this capability in adult transplants. Normal ABO-compatibility rules may be observed for all recipients. This means that anyone may receive a transplant of a type-O organ, and consequently, type-O recipients are one of the biggest beneficiaries of ABO-incompatible transplants. While focus has been on infant heart transplants, the principles generally apply to other forms of solid organ transplantation.
- United Network for Organ Sharing (UNOS) is the private, non-profit organization that manages the nation's organ transplant system under contract with the federal government. UNOS is involved in many aspects of the organ transplant and donation process: Managing the national transplant waiting list, matching donors to recipients 24 hours a day, 365 days a year. Maintaining the database that contains all organ transplant data for every transplant event that occurs in the U.S. Bring together members to develop policies that make the best use of the limited supply of organs and give all patients a fair chance at receiving the organ they need, regardless of age, sex, ethnicity, religion, lifestyle or financial/social status. Monitoring every organ match to ensure organ allocation policies are followed. Provides assistance to patients, family members and friends. Educates transplant professionals about their important role in the donation and transplant processes. Educating the public about the importance of organ donation
- There are 58 organ procurement organizations (OPOs) in the United States. OPOs are responsible for two main functions within their designated service area: increasing the number of registered donors, and 2) coordinating the donation process when actual donors become available. To increase donor sign-up, OPOs may implement any number of community outreach activities such as sponsoring advertising campaigns, programs in schools, worksites, or faith institutions, disseminating print and electronic materials, etc. When actual donors become available, OPOs evaluate the potential donors, check the deceased’s state donor registry, discuss donation with family members, contact the OPTN and run a match list, and arrange for the recovery and transport of donated organs. They also provide bereavement support for donor families and volunteer opportunities for interested individuals. OPOs employ a variety of staff including procurement coordinators, requestors, specialists in public relations, communication, and health education, as well as administrative personnel. OPOs must be certified by the Centers for Medicare and Medicaid Services (CMS) and abide by CMS regulations. By federal law, all OPOs must be members of the Organ Procurement and Transplantation Network (OPTN). All OPOs are members of the Association of Organ Procurement Organizations . Massachusetts New England Organ Bank Life Choice Donor Services (Franklin, Hampden, Hampshire Counties) Center for Donation and Transplant (Berkshire County)
- In order to be on the Wait List: Must be registered - Active list: conditions are favorable for transplant Inactive: conditions which temporarily rule out transplant (e.g. infection) Removal: describes patients who have been removed due to 1) personal choice, 2) they are too ill to survive the transplant, 3) are recovering adequate organ function, 40 have received a transplant (may be on multiple lists), or 5) have died What is the patient’s Stage of disease What are, if any, co-morbid conditions Thorough physical exam and psychological exam Maintain healthy life style
- The altruistic process of donation begins when people perform the simple act of indicating their consent to be a donor by enrolling in their state's donor registry. Most often this happens when obtaining or renewing a driver's license or by going on-line for those state registries that have an Internet registration capacity. Most people also tell their family they want to be a donor so their family member can support their decision when needed. Signing up to be a donor usually takes place many years before donation becomes a possibility.
- This may be familiar, especially if you have donated, or received blood or blood products. When discussing organ donation there actually three tests done to evaluate potential donors. They are blood type (like matching), crossmatch, and HLA testing. There are four different blood types (A, B, AB, and O) and the rules for blood type in transplantation are the same as those blood transfusion. An organ donor’s blood type must be compatible with an organ recipient's blood type.
- Blood types of the donor/patient pair. If the patient is of the ‘O’ blood type, then an ‘O’ donor is required. UNOS has a initiative called the Kidney Paired Program (KPD); This unique program offers designated donors:recipients an opportunity to receive an organ from a living donor. For example, someone wants to donate a kidney to you but your blood type is incompatible, or there is some other incompatibility. Also, imagine a second pair of people in the same situation; but, the second donor’s kidney IS compatible with yours and vice versa with your donor and the other recipient. By matching the four persons in this manner BOTH transplants can be done with a higher success rate!
- Earlier I mentioned there are three tests to evaluate organ donors. The Human leukocyte antigen (HLA) typing is used to match the recipient with a donor for bone marrow or cord blood transplant. HLA is a protein – or marker – found on most cells in your body. The immune system uses HLA markers to know which cells belong in our bodies, and which do not. Half of our HLA markers are inherited from our biological mother and half from our biological father. Siblings have 25%, or 1 in 4, chance of matching our HLA profile (the key term here is MATCH), IF you, if you have the same mother and father. It is highly unlikely that other family members will match us; aunts, cousins, half brothers, etc. About 70%, or 7 out of 10, patients who need a transplant do not have a suitable donor in their family. If an organ recipient candidate does not have a potential family donor, the transplant team may look for an unrelated donor, or cord blood unit for the patient. you on Be The Match Registry. When a search is done on the Be The Match Registry, it includes a search of more than 22.5 million potential adult donors and more than 601,000 cord blood units on lists from around the world.
- HLA matching is important because a close HLA match: Increases the likelihood of a successful transplant. Improves engraftment—when the donated cells start to grow and make new blood cells in you. Reduces the risk of complications after transplant, especially graft-versus-host disease (GVHD). GVHD is a potentially serious complication. GVHD occurs when the immune cells, which are part of the donated marrow or cord blood, attack your body.
- Rejection occurs if the donor organ does not perfectly match the recipient’s HLAs. The match between donor and recipient has to be at all three levels: ABO, Rh, HLA To combat activated T cells (which play a pivotal role in graft rejection), triple therapy is initiated for transplant recipients. Some drugs are used to block expansion of T cells – these reduce acute rejection and improve graft survival.
- Maintenance immunosuppression therapy is something which transplant recipients usually adhere for the rest of their lives. This combination includes a corticosteroid, a calcineurine inhibitor, and an antiproliferative. The concurrent administration of these three drugs have distinct combined effects on each individual. The balance of dosages can be altered to enhance the efficacy of the immunosuppression, but the most effective combination of prescriptions is unique for each individual patient. The goal of maintenance immunotherapy is to balance between underimmunosuppression (which result in graft rejection) and overimmunosuppression (which expose the patient to high risks of infection and other potentially fatal side effects). The various side effects of each drug must be considered, as well as potential interactions between drugs, especially those that cumulatively present significant risk factors to certain patients. Another variable for maintenance immunosuppression is the particular drugs prescribed.
- The introduction of cyclosporine 20 years ago to is one of the major breakthroughs of modern medicine. It has led to a significant improvement in the outcomes of organ trans-plantation. Way back in 1976 the biological properties of cyclosporine, the first immunosuppressive agent with a specific anti–T-lymphocyte activity, were recognized. Currently, cyclosporine is used for prevention of graft rejection in kidney, liver, heart, lung, and combined heart-lung transplantation. In addition, it found its place in bone marrow transplantation in prevention of graft-versus-host disease as well as in treatment of autoimmune conditions like psoriasis, atopic dermatitis, rheumatoid arthritis, and a variety of glomerular disorders
- Corticosteroids are an important part of maintenance therapy because of their anti-inflammatory and immunosuppressive effects. They inhibit cytokine production, circulation of lymphocytes, acid metabolites, and microvascular permeability. They also block T cell activation and proliferation. Prednisone and Methylprednisolone are two of the most commonly prescribed corticosteroids for organ transplant recipients. These drugs are non-specific and suppress the immune system in a global manner. Because this helps to induce a state of immune hyporesponsiveness, corticosteroids unfortunately have many harmful side effects for transplant patients. Corticosteroid use exemplifies the precarious balance between under- and over-prescription. Too much corticosteroid can cause hypertension, hyperglycemia, and opportunistic infection. Too little corticosteroid can result in graft rejection. Research has shown that a few months after transplantation, patients can be weaned off corticosteroids without increasing the frequency of rejection episodes. This decreases negative long-term medical complications.
- The final part of triple therapy includes antiproliferatives, such as Mycophenolate. This anti-mitotic drug inhibits DNA synthesis and the division of T cells. Before the advent of calcineurine inhibitors, antiproliferatives were the primary form of maintenance. These days, in maintenance therapy, its role is more general and supportive to the action of the calcineurine inhibitors. Several studies demonstrate that transplant patients can be gradually weaned off of antiproliferatives without a corresponding increase in graft rejection incidences. Lowering antiproliferative treatment is desirable over the course of long-term immunotherapy because the incidence of side effects, like thrombocytopenia, are reduced.
- The molecular mechanisms of graft rejection are based on recognition of foreign transplanted cells by the expression of polymorphic, codominant genes. These genes code for protein molecules which are found on the surfaces of cells called antigens. Due to polymorphism, it is rare to find a donor and recipient with matching surface antigens. Major histocompatibility complex (MHC) molecules are responsible for the most rapid rejection reactions. They are encoded by the MHC complex, a region of genes on chromosome 6 in human. These MHC molecules which present foreign peptides are in turn presented to recipient T-cells in two different ways, direct and indirect presentation.
- Inductive therapy refers to the prophylactic application of perioperative antibodies in addition to baseline immunosuppression. The goal of these drugs is to induce hyporesponsiveness in the organ recipient toward the transplanted organ in order to prevent early post transplant rejection. Ideally, only the T cells that respond to the donor antigen would be inhibited and the rest of the patient's immune system would remain fully functional. In all forms of immunosuppressive therapy, the applied dosages of drugs must balance efficacy of the immunosuppression and risk associated with general impairment of the immune system. The drugs must be strong enough to prevent rejection while protecting the patient from infection at the same time. This balance is complicated by the various interactions of multi-drug therapy; reactions can often be synergistic or lead to the up/down-regulation of drug metabolism.
- Despite the combined actions of maintenance triple immunotherapy, most transplanted organs do eventually fail. Immunotherapy is truly a treatment that delays the inevitability of graft rejection. However, when an acute rejection episode does finally occur, transplant patients still have good therapy options. In the vast majority of rejection episodes, the temporary treatment of high doses of corticosteroid is used to combat rejection by severely depressing the immune system. For those rejection episodes which are resistant to corticosteroid treatment, polyclonal and monoclonal antibodies are often employed as a rescue therapy.
- The rest of the discussion will center on our role, as nurses, and the care given as it relates to the unique aspects of the transplant recipient. The patient will be looked at in the acute stage (hospital), and after discharge, to home. The home, where our patient will be returning, has specific criteria; this is to protect the health, and promote recovery of the transplant patient. Transplants – the organs themselves – have some unique nursing care/assessment properties, and we will discuss this briefly. Last, infection and organ rejection, and the nurse’s role, will be discussed.
- Acute Phase (hospital): prior to surgery the nurse may be involved in answering patient questions, ensuring appropriate consents are signed, monitoring the patient’s condition, performing blood draws and monitoring the related lab values. After surgery the nurse will monitor the site of the surgery/the incision, administer antibiotics/IV, monitor for rejection, organ function (especially in the case of a deceased donor), for example a kidney receipt would have BUN and creatinine closely monitored. The qualities of a capable transplant unit nurse include being a good teacher: a transplant is a major life change. Incorporating teaching into the care of your patient is the best reinforcement of what the patient needs to learn. Because patient conditions can change rapidly the transplant unit nurse needs to have top assessment skills, and be able to modify his/her work flow to adjust for organ availability. Pain at the site of the transplant Feeling ill Flu-like symptoms Fever Weight change Swelling Decreased urine outpu
- Graft versus host disease (GvHD) is a condition that might occur after an allogeneic transplant. In GvHD, the donated bone marrow or peripheral blood stem cells view the recipient’s body as foreign, and the donated cells/bone marrow attack the body. Acute GvHD might occur once the donor's cells have engrafted in the transplant recipient. It might develop in the skin, liver, eyes, or gastrointestinal tract, and symptoms might appear within weeks after a transplant the diagnosis of a GvHD during a physical exam by observing certain symptoms and/or by evaluating the results of site biopsies and lab values.
- Let’s talk about caring for the transplant organ itself. Here are the priorities: Providing hemodynamic stabilization. When does this begin? At declaration of brain death. Brain death causes release of catecholamines from adrenals (Epinephrine and Norepinephrine) and this results in a hyper-dynamic state: Tachycardia, Elevated Cardiac Output. Vasoconstriction, Hypertension (called a Autonomic/Sympathetic Storm). the hypothalamus will fail which leads to impaired temperature regulation - hypothermia or hyperthermia; vasodilation without the ability to vasoconstrict or shiver (loss of vasomotor tone). This co-occurs with Pituitary Gland failure which controls the release ADH to conserve water. When ADH ceases to be produced Diabetes Insipidus results which can lead to hypovolemia and electrolyte imbalances. This leads to problems with the thyroid gland which stimulates the release of thyroid hormone. When the thyroid starts to malfunction we get Cardiac instability, Labile blood pressure, and Potential coagulation problems. Rule of 100’s: Maintain SBP > 100mmHG, keep HR < 100 BPM, Urinary Output > 100ml/hr., PaO2 > 100mmHg T4 PROTOCOL/ Bolus: 15 mg/kg Methylpred 20 mcg T4 (Levothyroxine) 20 units of Regular Insulin 1 amp D50W Infusion: 200 mcg T4 in 500 cc NS Run at 25 cc/hr (10 mcg/hr) Titrate to keep SBP >100 Monitor Potassium levels closely! appropriate intervention brain death is followed by severe injury to most other organ systems. Circulatory collapse will usually occur within 48hrs
- KIDNEY: Pain or tenderness over the transplant site, Fever, Flu-like symptoms such as chills, nausea, vomiting, tiredness, headache, dizziness, body aches and pains Little or no urine output, Sudden weight gain or swollen feet or ankles HEART: Fever, Shortness of breath, Flu-like symptoms such as chills, nausea, vomiting, diarrhea, tiredness, headache, dizziness, body aches and pains Difficulty sleeping on your back, Abnormal or irregular heartbeat, Weight gain or swelling, Decrease in blood pressure Liver: Yellow skin or eyes, Itching, Tea-colored urine or light-colored stool, Weight gain or swelling of the legs or stomach, Sudden tiredness Lung: Unexplained shortness of breath, Chest pain, Dry cough, General ill feeling, Decreased amount of air inhaled and decreased speed of air flow during a breath Pancreas: Increased blood sugar (glucose) measurements or sugar in the urine, Increased urination, Abdominal pain or fever or pain over the surgery site
