Laboratory Diagnosis of Jaundice
- 1. LABORATORY DIAGNOSIS OF JAUNDICE by Dr. Varughese George LABORATORY DIAGNOSIS OF JAUNDICE by Dr. Varughese George
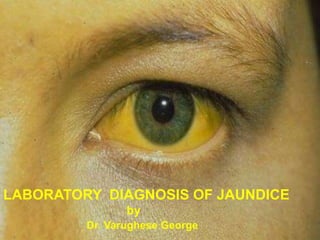
- 2. Jaundice Yellow discoloration of skin, sclera, and mucous membranes due to increased level of serum bilirubin. Jaundice becomes clinically evident when serum bilirubin level exceeds 2.0 mg/dl. (N- 1.2mg/dl) Causes Overproduction of bilirubin Defective hepatic bilirubin uptake Defective conjugation Defective excretion
- 3. Serum bilirubin levels Normal ◦ 0.2 to 0.8 mg/dL Unconjugated/free/indirect (bilirubin-albumin complex) ◦ 0.2 to 0.7 mg/dL Conjugated/direct: ◦ 0.1 to 0.4 mg/dL Latent jaundice: ◦ Above 1 mg/dL Clinical Jaundice: ◦ Above 2 mg/dL
- 5. Classification of Jaundice I. According to the main type of bilirubin increased in plasma: Predominantly unconjugated hyperbilirubinemia Predominantly conjugated hyperbilirubinemia Mixed (conjugated + unconjugated) hyperbilirubinemia Indirect or unconjugated bilirubin is > 85% of total; Direct or conjugated bilirubin is >50% of total Conjugated bilirubin is 20-50% of total Causes include Hemolysis Resorption of a large hematoma, Ineffective erythropoiesis (Thalassemia, Megaloblastic anemia) Physiologic jaundice of newborn. Congenital Gilbert’sSyndrome Crigler-Najjar syndrome. Causes include Hepatitis Cirrhosis Cholestasis Drug (anabolic steroids, oral contraceptives) Toxins Congenital Dubin-Johnson Syndrome Rotor syndrome. Causes include Viral Hepatitis Alcoholic Hepatitis
- 6. Classification of Jaundice II. According to etiology: Hemolytic Increased rate of RBC destruction Increased Hb breakdown to bilirubin in RES cells This exceeds the capacity of conjugation in liver. Hepatocellular Inability of hepatocytes to conjugate and/or excrete bilirubin. Obstructive Failure of excretion of conjugated bilirubin into the intestine, causing its regurgitation in circulation. Urinary and fecal urobilinogen are decreased,
- 7. Classification of Jaundice III. According to site of disease: Class of Jaundice Type of Bilirubin raised Causes Pre-hepatic or Hemolytic Unconjugated Hemolysis/Abnormal RBCs Antibodies drugs and toxins Thalessemia Hemoglobinopathies Hepatic or Hepatocellular Unconjugated and conjugated Viral hepatitis Toxic hepatitis Intrahepatic cholestasis Gilbert’s Syndrome Crigler-Najjar Syndrome Post-hepatic or Obstructive Conjugated Extrahepatic cholestasis Gallstones Tumors of the bile duct Carcinoma of pancreas Carcinoma of ampulla of Vater
- 8. DIFFERENTIAL DIAGNOSIS OF JAUNDICE Parameter Pre-hepatic Hepatocellular Obstructive Basic mechanism of raised bilirubin Hemolysis leading to excess production Deficient uptake, conjugation, or excretion by hepatocytes Deficient excretion due to obstruction of biliary tract Type of serum bilirubin increased Mainly unconjugated Unconjugated + Conjugated Mainly conjugated (>50%) Urine Bilirubin Absent Present Present Urine urobilinogen Increased Variable Decreased/Absent Prototype Hemolytic anemia Viral hepatitis Common duct stone Prothrombin time Normal Abnormal that isnt corrected with Vitamin K Abnormal that is corrected with Vitamin K Additional features Features of hemolysis on blood smear (reticulocytosis, low haptoglobin, low Hb Marked rise of serum ALT and AST Marked rise of serum ALP (>3 times normal)
- 9. Increased RBC turnover RBCs are the major source of bilirubin. Etiology Hemolytic anemia Ineffective erythropoiesis (thalassemia, megaloblastic anemia). Lab : increased unconjugated bilirubin. Chronic hemolytic anemia patients often develop pigmented bilirubinate gallstones
- 10. Physiological jaundice of the newborn Transient unconjugated hyperbilirubinemia observed in almost all newborns due to immaturity of the liver i.e deficiency of glucuronyl transferase leading to impaired conjugation during the first few days of life. First appears between 24-72 hrs of age Maximum intensity seen on 4-5th day in term & 7th day in preterm neonates. Doesn’t exceed 15 mg/dl Clinically undetectable after 14 days. Risk factors – Prematurity Hemolytic disease of the newborn (Erythroblastosis foetalis) Major complication is kernicterus especially in infants, in which increased levels of unconjugated lipid-soluble bilirubiin may cross the blood brain barrier and deposit in the basal gangllia, thus causing irreversible brain damage.
- 11. Congenital Hyperbilirubinemias Gilbert’s Syndrome Most common inherited cause of unconjugated hyperbilirubinemia. It is a familial, benign disease with autosomal dominant mode of inheritance. Affects 5% of general population. Mild deficiency or decreased hepatic levels of Bilirubin glucoronosyltransferase attributed to mutation in the encoding gene; polymorphisms in the gene may play a role in the variable expression of this disease Jaundice is mild and fluctuating, goes unnoticed for years; often related to stress/fasting/infection. Mildly elevated serum bilirubin is the sole abnormality; other LFTs are normal. Not associated with any morbidity.
- 12. Congenital Hyperbilirubinemias Crigler Najjar Syndromes Autosomal recessive disorder. Unconjugated hyperbilirubinemia. Type I - Serum bilirubin > 20 mg/dl Complete absence of Bilirubin UDP-glucoronosyltransferase1-A1 expression detected in liver tissue. Fatal due to kernicterus – causes rapid death in neonate. • Type II (Arias Syndrome) – • Serum bilirubin < 20mg/dl. • Reduced levels of detectable Bilirubin UDP-glucoronosyltransferase1- A1 expression in liver tissue owing to single base pair mutations. • Bile is pigmented instead of pale or dark as normal. • No risk of kernicterus.
- 13. Congenital Hyperbilirubinemias Dubin Johnson Syndrome • Benign autosomal recessive disorder. • Conjugated hyperbilirubinemia • Decreased hepatocellular bilirubin excretion due to a defect in the canalicular cationic transport protein. Gross : black pigmentation of the liver due to accumulation of polymerized epinephrine metabolites Lab - Bromosulphthalein excretion test is abnormal. • No clinical consequences
- 14. Congenital Hyperbilirubinemias Rotor Syndrome Autosomal recessive disorder. Conjugated hyperbilirubinemia. Decreased intraheptic binding. Similar to Dubin-Johnson but without liver pigmentation. Bromosulphthalein test is normal. No clinical consequences.
- 15. Other Hyperbilirubinemias Biliary Tract Obstruction Etiology - Gall stones Tumors (pancreatic, gall bladder and bile duct) Strictures Parasites (Liver flukes – Clonorchis sinensis) Presentation – Jaundice & icterus. Pruritis due to raised plasma levels of bile acids. Abdominal pain, fever and chills Dark urine (bilirubinuria) Pale clay colored stools Laboratory Diagnosis – Increased conjugated bilirubin. Increased alkaline phosphatase. Increased 5’ nucleotidase.
- 16. Other Hyperbilirubinemias Primary biliary cirrhosis Chronic liver disease of unknown etiology probably autoimmune characterised by inflammation & granulomatous destruction of intrahepatic bile ducts. Males: Females = 1:10, age – 30-65 yrs. Presentation : middle-aged women with obstructive jaundice: xanthomas, xanthelasmas, increased serum cholesterol, fatigue, cirrhosis. Laboratory Diagnosis - Increased conjugated bilirubin Increased alkaline phosphatase Increased 5’ nucleotidase. Antimitochondrial Antibody Most people have another autoimmune disease. Microscopy : Lymphocytic & granulomatous destruction of interlobular bile ducts.
- 17. Other Hyperbilirubinemias Primary sclerosing cholangitis Chronic liver disease of unknown etiology characterized by segmental inflammation & fibrosing destruction of intra-& extrahepatic bile ducts. Males: Females = 2:1, age – 20-40yrs; most associated with ulcerative colitis. Presentation – similar to Primary Biliary Cirrhosis. Microscopy – Periductal chronic inflammation. Concentric fibrosis around bile ducts. Segmental stenosis of the bile ducts. Beaded appearance of bile ducts on cholangiogram. ANCA is a Marker for Primary Sclerosing Cholangitis.
- 19. Evaluation of acute hepatocellular injury
- 20. Classification of Liver Function Tests Group I: Markers of liver dysfunction Serum bilirubin: total, conjugated and unconjugated Urine: bile pigments, bile salts and urobilinogen Total protein, serum albumin and albumin/globulin ratio Prothrombin Time Group II: Markers of hepatocellular injury Alanine aminotransferase (ALT) Aspartate aminotransferase (AST) Group III: Markers of cholestasis Alkaline phosphatase (AKP) γ- glutamyl transferase (GGT) 5’-nucleotidase (5’-NT)
- 21. Hepatocellular Locations of Enzymes Alanine aminotransferase (ALT) and the cytoplasmic isoenzyme of aspartate aminotransferase (ASTc) are found primarily in the cytosol. With membrane injury as in viral or chemically-induced hepatitis, these enzymes are released and enter the sinusoids, raising plasma AST and ALT activities. Mitochondrial aspartate aminotransferase (ASTm) is released primarily with mitochondrial injury, as caused by ethanol as in alcoholic hepatitis. Alkaline phosphatase (ALP) and Gamma-glutamyltransferase (GGT) are found primarily on the canalicular surface of the hepatocyte. Bile acids accumulate in cholestasis and dissolve membrane fragments, releasing bound enzymes into plasma. GGT is also found in the microsomes, represented as rings in the figure; microsomal enzyme-inducing drugs, like phenobarbital and dilantin, can also increase GGT synthesis and raise plasma GGT activity.
- 22. INTERPRETATION OF LIVER FUNCTION TESTS Typical LFT profile in hepatocellular disease Marked elevation of AST and ALT (usually >500 IU) Mild increase of ALP (<3 times normal) Hyperbilirubinemia, if present, is of both conjugated and unconjugated type Typical LFT profile in cholestatic jaundice Marked elevation of ALP (>3 times normal) Elevation of GGT and 5’- NT. Mild or no increase of ALT and AST (usually <200 IU). Elevation of conjugated bilirubin
- 23. Estimation of serum bilirubin Spectrophotometry used for measurement of total serum bilirubin in newborns and infants (<3 months of age). Concentration of serum bilirubin is directly proportional to its absorbance in a spectrophotometer at 454 nm. This method cannot be used in older children and adults because their sera may also contain carotene and other pigments, which absorb light at the same wavelength. In newborns, other pigments are absent. Diazo Method Direct bilirubin (Conjugated bilirubin): It reacts directly with diazo reagent. It consists of monoconjugated bilirubin, diconjugated bilirubin, and bilirubin tightly bound to albumin (delta bilirubin). Indirect bilirubin (Unconjugated bilirubin): It reacts with diazo reagent in the presence of alcohol. It consists of bilirubin bound to albumin. It is calculated as ‘total bilirubin minus direct bilirubin’.
- 24. Serum Aminotransferases Serum aminotransferases (AST/ALT) are the sensitive markers of acute hepatocellular injury. Serum alanine aminotransferase or ALT (formerly called serum glutamic-pyruvic transaminase or SGPT) is a cytosolic enzyme. Serum aspartate aminotransferase or AST (formerly called serum glutamic-oxaloacetic transaminase or SGOT) is both cytosolic and mitochondrial. When necrosis or death of cells containing these enzymes occurs, aminotransferases are released into the blood and their concentration in blood increases whose level correlates with extent of tissue damage. Most marked elevations of ALT and AST (>15 times normal) are seen in acute viral hepatitis, toxin-induced hepatocellular damage (e.g. carbon tetrachloride), and centrilobular necrosis due to ischemia (congestive cardiac failure). Moderate elevations (5-15 times) occur in chronic hepatitis, autoimmune hepatitis, alcoholic hepatitis, acute biliary tract obstruction, and drug-induced hepatitis. Mild elevations (1-3 times) are seen in cirrhosis, nonalcoholic steatosis, and cholestasis. Increase of AST and ALT is much more in hepatocellular jaundice (>500 units/ml) than in cholestatic jaundice (<200 units/ml). ALT and AST are elevated in acute viral hepatitis even before the appearance of jaundice. Persistence of elevated ALT and AST beyond 6 months in a case of hepatitis indicates development of chronic hepatitis In massive liver necrosis, aminotransferase levels gradually decrease. Normal ALT:AST ratio is 0.7 to 1.4.
- 25. Serum Alkaline Phosphatase (ALP) In the liver, ALP, GGT, and 5’-NT are located normally on canalicular surface of hepatocytes. Serum ALP levels are increased in most cases of cholestatic type of jaundice and hence helps in differentiating it from hepatocellular jaundice. Hepatobiliary causes of increased alkaline phosphatase include – Bile duct obstruction (cancer of head of pancreas/stone in common bile duct/stricture of bile duct/ biliary atresia) Primary biliary cirrhosis Primary sclerosing cholangitis Infiltrative diseases of liver - Granulomatous diseases like tuberculosis/sarcoidosis - Amyloidosis - Cysts - Primary/secondary cancer. Serum ALP levels are also raised in diseases of bone and pregnancy.
- 26. Serum γ-glutamyl Transferase (GGT) Relatively high levels of this enzyme are present in liver, pancreas, kidney & prostate. Estimation of this enzyme is particularly useful in following liver diseases: Alcoholism - Increased enzyme activity is present in alcoholism, and is a helpful clue in suspected cases of occult alcoholism. Cholestasis: - Elevation of GGT generally parallels that of ALP and 5’-NT in liver diseases like primary biliary cirrhosis or sclerosing cholangitis. Recovery in acute hepatitis: - Serum GGT is the last enzyme to return to normal following acute hepatitis and its normalization is indicative of a favourable outcome.
- 27. 5’-nucleotidase (5’-NT) 5’-NT is present in liver as well as in various other tissues. It is located mainly along the cell membrane, similar to ALP and GGT. Estimation of 5’-NT is helpful in deciding whether increased ALP is due to liver disease or due to increased osteoblastic activity in growing children.
- 28. Serum Albumin Serum albumin is a sensitive but nonspecific test for liver disease Albumin is synthesized exclusively in liver and constitutes about 60% of total proteins in serum important investigation in liver disease Half-life of albumin is about 20 days. In acute liver disease (e.g. viral hepatitis), there is little change in albumin level., whereas it is low in chronic liver disease (cirrhosis) and correlates with synthetic capacity of hepatocytes it is helpful in following progression of cirrhosis. Fall in serum albumin level correlates with severity of ascites. Serum albumin is estimated by bromocresol green which binds selectively and tightly to it thus imparting a blue color Absorbance (in a spectrophotometer at 632 nm) is directly proportional to concentration of albumin. Causes of decreased serum albumin: Decreased intake: malnutrition. Decreased absorption: malabsorption syndromes. Decreased synthesis: liver disease, chronic infections. Increased catabolism: thyrotoxicosis, fever, malignancy, infections. Increased loss: nephrotic syndrome, severe burns, protein-losing enteropathies, ascites Increased blood volume: pregnancy, congestive cardiac failure.
- 29. Prothrombin Time (PT) Prothrombin Time(PT) measures three out of four vitamin K-dependent factors (II, VII, and X) and is prolonged in hepatocellular disease and in obstructive jaundice. Deficient synthesis of Vitamin K dependent factors occurs in hepatocelllular jaundice. In obstructive jaundice, vitamin K (a fat-soluble vitamin) cannot be absorbed due to the absence of bile in the intestine. Intramuscular injection of vitamin K corrects prolonged PT in obstructive jaundice but not in hepatocellular jaundice. In acute fulminant liver failure, marked prolongation of PT is an unfavourable prognostic sign.
- 30. Bile pigments in Urine The main bile pigments are bilirubin and biliverdin. Bilirubin is converted to non-reactive biliverdin on exposure to light (daylight or fluorescent light) and on standing at room temperature. Biliverdin cannot be detected by tests that detect bilirubin. Therefore fresh sample that is kept protected from light is required. Presence of bilirubin in urine indicates conjugated hyperbilirubinemia (obstructive or hepatocellular jaundice) as only conjugated bilirubin is water-soluble. Bilirubin in urine is absent in hemolytic Jaundice because unconjugated bilirubin is water-insoluble. Urine Test Hemolytic Jaundice Hepatocellular Jaundice Obstructive Jaundice Bile pigments Absent Present Present
- 31. Detection of bile pigments in urine Fouchet’s test 2.5 ml of 10% of barium chloride is mixed with 5 ml of fresh urine in a test tube. A precipitate of sulphates appears to which bilirubin is bound (barium sulphate-bilirubin complex). Filter to obtain the precipitate on a filter paper followed by an addition of 1 drop of Fouchet’s reagent(25g of CCl3COOH, 10ml of 10% FeCl3 & distilled water 100ml) to it. Immediate development of blue-green color around the drop => presence of bilirubin.
- 32. Detection of bile pigments in urine Foam Test 5ml of urine in test-tube is shaken and yellow foam => presence of bilirubin. Gmelin’s test: 3 ml of concentrated HNO3 is added to an equal quantity of urine in a test tube and shaken gently. Play of colors(yellow, red, violet, blue, and green) => +ve test. Lugol iodine test: 4 ml of Lugol iodine solution (I 1gm, KI 2 gm, and distilled water to make 100 ml) is added to 4 drops of urine in a test tube and mixed by shaking and green color => +ve test. Reagent strips or tablets impregnated with diazo reagent: Tests based on reaction of bilirubin with Diazo reagent. Color change is proportional to the concentration of bilirubin. Tablets (Ictotest) detect 0.05-0.1 mg of bilirubin/dl of urine. Reagent strip tests are less sensitive (0.5 mg/dl).
- 33. Bile salts in urine Bile salts are salts of four different types of bile acids: cholic deoxycholic chenodeoxycholic lithocholic. Bile acids combine with glycine or taurine to form complex salts or acids. Bile salts enter the small intestine through the bile and act as detergents to emulsify fat and reduce the surface tension on fat droplets so that enzymes (lipases) can breakdown the fat. In the terminal ileum, bile salts are absorbed and enter in the bloodstream from where they are taken up by the liver and re- excreted in bile (enterohepatic circulation). Bile salts along with bilirubin can be detected in urine in cases of obstructive jaundice in which bile salts and conjugated bilirubin regurgitate into blood from biliary canaliculi (due to increased intrabiliary pressure) and are excreted in urine.
- 34. Detection of bile salts in urine Hay’s surface tension test The property of bile salts to lower the surface tension is utilized in this test . Fresh urine at room temperature taken in a conical glass tube is sprinkled on the surface particles of sulphur. If bile salts are present, sulphur particles sink to the bottom because of lowering of surface tension by bile salts. If sulphur particles remain on the surface of urine, bile salts are absent. Thymol (used as a preservative) gives false positive test.
- 35. Urobilinogen Conjugated bilirubin excreted into the duodenum through bile is converted by bacterial action to urobilinogen in the intestine. Major part is eliminated in the feces. A portion of urobilinogen is absorbed in blood, which undergoes recycling (enterohepatic circulation); A small amount, which is not taken up by the liver, is excreted in urine. Urobilinogen is colorless; upon oxidation it is converted to urobilin, which is orange-yellow in color. Normally about 0.5-4 mg of urobilinogen is excreted in urine in 24 hours. Therefore, a small amount of urobilinogen is normally detectable in urine. A 2-hour post-meal sample is often preferred as urinary excretion of urobilinogen shows diurnal variation with highest levels in afternoon. Urine Test Hemolytic Jaundice Hepatocellular Jaundice Obstructive Jaundice Urobilinogen Increased Increased Absent
- 36. Urobilinogen Causes of Increased Urobilinogen in Urine Hemolysis: Excessive destruction of red cells leads to hyperbilirubinemia and therefore increased formation of urobilinogen in the gut. Hemorrhage in tissues: There is increased formation of bilirubin from destruction of red cells. Causes of Decreased Urobilinogen in Urine Obstructive jaundice In biliary tract obstruction,delivery of bilirubin to the intestine is restricted and very little or no urobilinogen is formed. This causes stools to become clay-colored. Reduction of intestinal bacterial flora: This prevents conversion of bilirubin to urobilinogen in the Intestine; observed in neonates and following antibiotic treatment.
- 37. Detection of Urobilinogen in urine Ehrlich’s aldehyde test: 0.5 ml Ehrlich’s reagent (pdimethylaminobenzaldehyde) is added to a 5ml fresh 2 hr postprandial sample of urine. If urobilinogen present, it ll reach with Ehrlich’s reagent and produce a pink color. Intensity of color developed depends on the amount of urobilinogen present. Development of pink color normal amount of urobilinogen. Development of dark red color increased amount of urobilinogen. Watson-Schwartz’s Test Test distinguishes between urobilinogen and porphobilinogen which gives similar results in Ehrlich’s test. 1-2ml chloroform is added to the sample, shaken for 2 mins & allowed to stand. Pink color in the chloroform layer indicates presence of urobilinogen, while pink coloration of aqueous portion indicates presence of porphobilinogen Reagent strip method: Method is specific for urobilinogen. Test area is impregnated with either p-dimethylaminobenzaldehyde or 4-methoxybenzene diazonium tetrafluoroborate False -ve reaction • UTI (nitrites oxidize urobilinogen to urobilin) •Antibiotic therapy (gut bacteria which •produce urobilinogen are
