Management of apical lesions
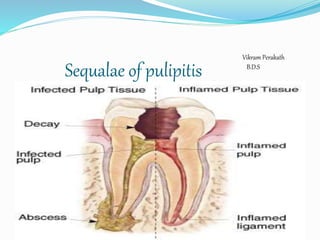
- 1. Sequalae of pulipitis Vikram Perakath B.D.S
- 2. Pulpitis Pulp becomes infected by Carious exposure, Leaking restorations , Dentinal tubules , Fractures or cracks. Leading to an inflammatory response(i.e.chemotaxis,enzymatic breakdown with release of antigens)
- 3. Antigens in the surrounding tissue. Leads to an immune response from the tissue-antibodies. The response destroys much of the peripical tissue leading to the formation of various types of apical periodontal lesions.
- 4. SEQUALE OF PULPITIS Necrotic pulp Apical periodonti tis Acute periapical abscess Chronic periapaical granuloma Periapical cyst Osteomyelitis Cellulitis Periostitis Abscess
- 5. Acute chronic Apical Periodontitis Periapical abscess (Acute chronic) Periapical granuloma Osteomyelitis (Acute Chronic) Periodontal cyst Periostitis Cellulitis Abscess Pulpitis Acute Chronic Focal Diffuse Interrelationships of periapical infection
- 6. Apical periodontitis It is the inflammation of the periodontal ligament around the root apex. The common causes are Spread of Infection following pulp necrosis Occlusal Trauma, Chemical irritation(Overextended R.C.T medicaments) There are two types-Acute Apical Periodontitis(AAP) Chronic Apical Periodontitis(CAP)
- 7. Acute periodontitis Previous h/o pulpitis Thermal changes do not induce pain Tooth is elevated from the socket with tenderness Chronic periodontitis •AKA periapical granuloma •Sequale of pulpitis or acute periapical periodontitis. •Tooth involved is usually non-vital & maybe tender
- 8. Treatment Acute periodontitis- If there is occlusal trauma-selective grinding If pulpally involved-R.C.T/Extraction Chronic periodontitis(Periapical granuloma)- Extraction of involved teeth R.C.T/R.C.T with apisectomy If left untreated it will transform intoApical periodontal cyst
- 9. Apical granuloma A “granuloma” is, literally, a mass made up of granulation tissue. Most common type of pathologic radiolucencies. It is the result of a successful attempt by the periapical tissues to neutralize and confine the irritating toxic products that are escaping from the root canal. More inflammation at the center of the lesion The Periphery of the lesion shows fibrosis (healing)
- 10. Radiographically-well-circumscribed radiolucency somewhat rounded and surrounding the apex of the tooth It is difficult to differentiate from a radicular cyst radiographically.Both have large, well defined radiolucency with radiopaque (sclerotic) border.
- 11. Apical periodontal cyst(AKA Radicular cyst,Periapical cyst,Dental cyst,Root end cyst) It is usually a sequale of Periapical Granuloma It is a true cyst,since the lesion consists of a pathological cavity lined by epithelium and is often fluid filled. The epithelium is from cell rests of Malassez. Clinical features: Usually asymptomatic Most common in maxillary anteriors. May undergo acute exacerbation of the inflammatory process and develop rapidly into an abscess,then cellulitis.
- 12. Radiographic features: A thin radiopaque line around the periphery of radiolucent area seen, indicating a reaction of the bone to the slowly growing mass Cannot differentiate between Granuloma and cyst radiographically.Diagnosis is based on histologic examination. Treatment : Extraction of involved tooth & curettage of socket Rct with apisectomy
- 13. Periapical abscess(AKA Dentoalveolar abscess,Alveolar abscess) It is an acute or chronic suppurative processs of the periapical region. It is a sequalae of A.A.P or a periapical granuloma . Phoenix abscess is an acute exacerbation of chronic periapical lesion. Chronic abscess is an asymptomatic,well-circumscribed area of suppuration that shows little tendency to spread from local area. Clinical features : Intially- Tenderness,which is relieved by application of pressure. Later-Extreme pain & slight extrusion from socket. Rapid extension to adjacent marrow spaces may occur,resulting in osteomyelitis.
- 14. Radiographically: Ill-defined radiolucent area at the apex of the tooth. Treatment: Drainage of abcess: Opening the pulp chamber Extraction If left untreated it can lead to osteomyelitis, cellulitis.
- 15. Osteomyelitis Inflammation of bone & its marrow contents. Though the dividing line between osteomyelitis and an abscess is unclear,osteomyelitis is usually reserved for infections that spread through the bone to a larger extent. Predisposing factors : Fracture due to trauma,RTA, radiation damage, ostopetrosis,gun-shot wounds,Paget’s disease. Systemic conditions: DM, sickle cell anemia, chronic alcoholism,malnutrition,acute leukemia.
- 16. Acute suppurative osteomyelitis It is a serious sequale of periapical infection resulting in the diffuse spread of infection throughout the medullary spaces with subsequent necrosis of varible amount of bone. Common causes: Dental infection Abscess(if virulent and not walled off) Acute exacerbation of a granuloma or cyst Clinical features: In the maxilla,tends to be localised to involved tooth but in the mandible it is more diffuse & widespread. Pain, trismus, paresthesia of lip, elevation of temp,regional lymphadenopathy,loose and tender involved teeth Wbc is elevated, pus from gingival margin.
- 17. Radiographically: Changes can be seen after 1-2 weeks.Ill-defined margins & moth eaten appearance. Treatment : Debridement , Drainage & Drugs(antibiotic therapy) Surgical removal for lesions with large sequestrum. If left untreated,may proceed to Periostitis,soft-tissue abscess or cellulitis.
- 18. Chronic suppuartive osteomyelitis Clinical features are similar to those of acute osteomyelitis,except that all signs and symptoms are milder. Occurs in people with high tissue reactivity. Commonly occurs in children & young adults,in the mandibular 1st molar. There maybe no clinical symptoms other than mild pain associated with an infected pulp. Path of entry of infection maybe diffuse periodontal disease. Commonly occurs in older people,especially in edentulous mandibular jaws. Often there are no clinical features,sometimes due to acute exarcebation of chronic infection,there is vague pain,unpleasant taste,mild suppuration,fistula formation to mucosal surface. Chronic Focal Sclerosing Osteomyelitis(Condensing osteitis) Chronic Diffuse Sclerosing Osteomyelitis
- 19. Radiographically: Well circumscribed radio-opaque mass of sclerotic bone extending below the root apex of the roots. Intact lamina dura P.D.L ligament space widening(to diff. From benign cementoblastoma) Diffuse,patchy,sclerosis of bone,often described as “cotton-wool” appearance. Treatment: Affected tooth is extracted or treated endodontically. Sclerotic bone,not attached to tooth,remains after extraction. Treatment is difficult.Conservative approach is most reasonable. Teeth involved in sclerotic lesion to be extracted.
- 20. Chronic Osteomyelitis with Proliferative Periostitis(Garre’s chronic non-suppurative sclerosing osteitis,periostitis ossificans) Shows focal gross thickening of the periosteum,with peripheral reactive bone formation due to infection or irritation. Clinical features: Almost exclusive to mandible,in premolar and molar region,of children and young adults. Presents as pain in the jaw with a bony hard swelling on the outer surface of the jaw.
- 21. Radiographically: Occlusal radiograph shows focal overgrowth of bone on the outer surface of the cortex,which maybe described as duplication of the cortical layer of bone. Intraoral radiograph will reveal a carious tooth opposite the hard bony mass. Treatment: Extraction or R.C.T of infected tooth. Biopsy to confirm diagnosis.
- 22. References Shafer’s Textbook of Oral Pathology(7th edition)
- 24. Non Surgical management of apical lesions The aim of non-surgical root canal therapy is the elimination of infection from the root canal and the prevention of re-infection by root filling Periapical lesions develop as sequelae to pulp disease. They often occur without any episode of acute pain and are discovered on routine radiographic examination.
- 25. All inflammatory periapical lesions should be initially treated with conservative nonsurgical procedures. The ultimate goal of endodontic therapy should be to return the involved teeth to a state of health and function without surgical intervention.
- 26. METHODS FOR NONSURGICAL MANAGMENT OF PERIAPICAL LESIONS 1. Conservative root canal treatment without adjunctive therapy 2. Decompression technique 3. Active nonsurgical decompression technique 4. Aspiration and irrigation technique 5. Method using calcium hydroxide 6. Lesion sterilization and repair therapy 7. Apexum procedure
- 27. Conservative root canal treatment without adjunctive therapy Instrumentation should be carried 1 mm beyond the apical foramen. Establishes drainage and relieves pressure. Once the drainage stops,fibroblasts begin to proliferate and deposit collagen; this compresses the capillary network, and the epithelial cells are thus starved, undergo degeneration, and are engulfed by the macrophages.
- 28. Causes transitory inflammation and ulceration of the epithelial lining resulting in resolution of the cyst. Weekly debridement and drying of the canals over a period of two to three weeks, followed by obturation has led to a complete resolution of lesions by 12 to 15 months.
- 29. Decompression technique The placement of a drain into the lesion, daily irrigation using 0.12% chlorhexidine, periodic length adjustment, and maintenance of the drain, for various periods of time Advantages: Simple procedure,minimal damage,easily tolerated. Contraindicated: Large dental granulomas or any solid cellular lesion.
- 30. Active nonsurgical decompression technique This technique uses the Endo-eze vacuum system (Ultradent,Salt Lake, Utah) to create a negative pressure, which results in the decompression of large periapical lesions. The high-volume suction aspirator is connected to a micro 22- gauge needle, which is inserted in the root canal and activated for 20 minutes, creating a negative pressure, which results in aspiration of the exudate. When the drainage partially stops, the access cavity is closed with temporary cement,which helps in maintaining bacterial control. Advantage: Minimally invasive, as the entire procedure is done through the root canal and causes less discomfort for the patient
- 31. Aspiration and irrigation technique Aspiration of the cystic fluid from the periapcial lesion using a bucco-palatal approach. An 18-gauge needle attached to a 20 ml syringe is used to penetrate the buccal mucosa and aspirate the cystic fluid. A second syringe filled with saline is inserted through the buccal wound and passed out through the palatal tissue creating a pathway for the escape of the irrigant. Disadvantage: Buccal and palatal wounds that may cause discomfort to the patient.
- 32. Method using calcium hydroxide Calcium hydroxide has bactericidal effects. It creates favourable conditions for periapical repair and stimulates hard tissue formation. The four- fold effect of Ca(OH)2: (a) anti-inflammatory activity, (b) neutralization of acid products, (c) activation of the alkaline phosphatase, and (d) antibacterial action Calcium hydroxide is used as an antibacterial agent for only 15 days, following which it is irrigated out of the canal using sodium hypochlorite.
- 33. Lesion sterilization and repair therapy The Cariology Research Unit of the Niigata University School of Dentistry has developed the concept of ‘Lesion Sterilization and Tissue Repair (LSTR)’ therapy that uses a triple antibiotic paste of ciprofloxacin, metronidazole,and minocycline, for disinfection of oral infectious lesions. Repair of damaged tissues can be expected if lesions are disinfected. The combination of drugs has been shown to penetrate efficiently through dentine from the prepared root canals. The commercially available drugs are powdered and mixed in a ratio of 1:3:3 (3 Mix) and mixed either with macrogol-propylene glycol (3 Mix-MP) or a canal sealer(3 Mix-sealer) Disadvantage is tooth discoloration induced by minocycline.
- 34. Apexum procedure The Apexum procedure uses two sequential rotary devices, the Apexum NiTi Ablator and Apexum PGA Ablator (Apexum Ltd, Or Yehuda, Israel), designed to extend beyond the apex and mince the periapical tissues on rotation in a lowspeed handpiece, followed by washing out the minced tissue. Significantly faster periapical healing is noted with this technique.
- 35. Surgical management of apical lesions In the following slides I will talk about the principles of management of apical lesions or odontogenic deep fascial space infections,as laid down by The late Dr. Larry Peterson.
- 36. There are eight sequential steps that are to be followed with thoroughness and good judgment to ensure a high level of care for these occasionally life-threatening infections.
- 37. The eight steps in the management of odontogenic infections are as follows: 1. Determine the severity of infection. 2. Evaluate host defenses. 3. Decide on the setting of care. 4. Treat surgically. 5. Support medically. 6. Choose and prescribe antibiotic therapy. 7. Administer the antibiotic properly. 8. Evaluate the patient frequently.
- 38. OR 1.Severity of infection 2.Host defenses 3.Care setting 4.Surgical treatment 5. Medical support 6. Prescribe antibiotics 7.Administer antibiotics properly 8.Evaluate Frequently
- 39. Step 1: Determine the Severity of Infection Three major factors must be considered in determining the severity of an infection of the head and neck: 1.Anatomic location 2.Rate of progression 3.Airway compromise.
- 40. Anatomic Location The anatomic spaces of the head and neck can be graded in severity by the level to which they threaten the airway or vital structures, such as the heart and mediastinum or the cranial contents.
- 41. Buccal Infraorbital low severity Vestibular Subperiosteal
- 42. Masticatory space: Submasseteric Pterygomandibular, Superficial and Deep temporal spaces Perimandibular spaces: Submandibular Submental Sublingual Moderate severity
- 43. Lateral pharyngeal Retropharyngeal The danger space highseverity Mediastinum Cavernous sinus thrombosis
- 44. The Danger space It is found between the buccopharnygeal fascia and alar fascia,posterior to retropharygeal space,it gets its common name from the risk that an infection in this space can spread directly to the thorax, it is sometimes also referred to as the Alar space.)
- 45. A severity score (SS) was devised that assigned a numerical value of 1 to 4 for involvement of each of the anatomic spaces involved,be it low(1), moderate(2), severe(3) or extreme severity(4), respectively.
- 46. Severity score = 1 (low risk to airway or vital structures) Vestibular Subperiosteal Space of the body of the mandible Infraorbital Buccal Severity score = 2 (moderate risk to airway or vital structures ) Submandibular Submental Sublingual Pterygomandibular Submasseteric Superficial temporal Deep temporal (or infratemporal)
- 47. Severity score = 3 (high risk to airway or vital structures) Lateral pharyngeal Retropharyngeal Pretracheal Severity score = 4 (extreme risk to airway or vital structures) Danger space Mediastinum Intracranial infection
- 48. Rate of Progression Characteristi c Inoculation Cellulitis Abscess Duration 0–3 3–7 Over days days 5 days Pain Mild–moderate Severe Moderate–severe and generalized Size Small Large Small Localization Diffuse Diffuse Circumscribed Palpation Soft,doughy Hard, Fluctuant,
- 49. Necrotising fasciitis A special note should be made of an especially rapidly progressive infection called necrotizing fasciitis. It is a rapidly spreading infection that follows the platysma muscle down the neck and onto the anterior chest wall.
- 50. Airway Compromise The most frequent cause of death in odontogenic infections is airway obstruction. Complete airway obstruction is a surgical emergency. Insufficient or absent air movement inspite of inspiratory efforts will be apparent.Check O2 saturaltion levels. One brief attempt at endotracheal intubation maybe made,but a direct surgical approach to the airway by cricothyroidotomy or tracheotomy is more predictably successful. Infection in the region of surgical airway access is not a contraindication to an emergency cricothyroidotomy or tracheotomy.
- 51. Step 2: Evaluate Host Defenses Immune System Compromise: The medical conditions that can interfere with proper function of the immune system Diabetes Steroid therapy Organ transplants Malignancy Chemotherapy Chronic renal disease Malnutrition Alcoholism End-stage AIDS
- 52. Other conditions that impair immune function: Malnutrition, Alcoholism, Chronic renal disease.
- 53. Systemic Reserve The host response to severe infection can place a severe physiologic load on the body. An elevated temperature at an advanced age is not only a sign of a particularly severe infection, but also of decreased cardiovascular and metabolic reserve, due to the demands placed on the elderly patient’s physiology by the high grade long standing fever associated with the infection. Evaluation of W.B.C count is important in determining the severity of infection as well as in estimating the length of hospital stay.
- 54. The physiologic stress of a serious infection can disrupt previously well established control of systemic diseases such as diabetes, hypertension, and renal disease. An otherwise mild or moderate infection may be a significant threat to the patient with systemic disease, and the surgeon should be careful to evaluate and manage concurrent systemic diseases in conjunction with direct management of the infection
- 55. Step 3: Decide on the Setting of Care Admission of a patient to hospital is indicated when: Temperature > 101°F (38.3°C) Dehydration -This can be assessed by elevated urine specific gravity (over 1.030) or an elevated blood urea nitrogen (BUN). Infections in deep spaces that have a severity score of 2 or greater, can hinder access to the airway for intubation by causing trismus, directly compress the airway by swelling, or threaten vital structures directly and indicates hospital admission. Need for general anesthesia Need for inpatient control of systemic disease
- 56. Step 4: Treat Surgically Secure the airway Incision and drainage Straight forward treatments, such as removal of the involved teeth, intraoral incision and drainage, and empiric antibiotic therapy, are almost always successful. Culture and Sensitivity Testing if economically viable.
- 57. Step 5: Support Medically Hydration -Reestablishment of electrolyte balance. A 70 kg patient with a fever of 102.2°F would have a daily fluid requirement of about 3,100 mL. Nutrition, Control of fever- Initial temperature- Above 39.4’C or 103’F fever,it can become destructive by increasing metabolic and cardiovascular demands, beyond physiologic reserve capacity of the patient. Administration of acetaminophen or aspirin
- 58. Step 6: Choose and Prescribe Antibiotic Therapy Severity of Infection Antibiotic of Choice Outpatient Penicillin Clindamycin Cephalexin In case of penicillin allergy: Clindamycin Moxifloxacin Metronidazole alone Inpatient Clindamycin Ampicillin + metronidazole Ampicillin + sulbactam In case of Penicillin allergy: Clindamycin Moxifloxacin Metronidazole alone
- 59. Step 7: Administer the Antibiotic Properly The tissue-serum level of antibiotics determines their effectiveness. Orally administered antibiotics achieve much lower serum levels at a slower rate than when they are injected directly into the vascular system intravenously.
- 60. Step 8: Evaluate the Patient Frequently In outpatient infections that have been treated by tooth extraction and intraoral incision and drainage, The most appropriate initial follow-up appointment is usually at 2 days postoperatively for the following reasons: 1. Usually the drainage has ceased and the drain can be discontinued at this time. 2. There is usually a discernible improvement or deterioration in signs and symptoms.
- 61. For odontogenic deep fascial space infections that are serious enough for hospitalization, daily clinical evaluation and wound care are required for at least two to three days. If there are no signs of clinical improvement in these 2-3 days, then it may be necessary to begin an investigation for possible treatment failure. One of the best methods of re-evaluation is the postoperative C.T scan.
- 62. Severe odontogenic infections can be the most challenging cases that an oral and maxillofacial surgeon will be called on to treat. Often the patient with a severe odontogenic infection has significant systemic or immune compromise, and the constant threat of airway obstruction due to infections in the maxillofacial region raises the risk of such cases severely
- 63. The eight steps in the treatment of severe odontogenic infections, first outlined by Dr. Larry Peterson, remain the fundamental guiding principles that oral and maxillofacial surgeons must use in successful management of these cases. The surgeon’s mind must always remain open to the possibility of treatment failure, an error in initial diagnosis, antibiotic resistance, and previously undiagnosed medically compromising conditions.
- 64. References Nonsurgical management of periapical lesions- Marina Fernandes, Ida de Ataide,Department of Conservative Dentistry and Endodontics, Goa Dental College and Hospital, Bambolim, Goa - 403 601, IndiaJournal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4 Peterson's Principles of Oral and Maxillofacial Surgery 2nd Ed 2004.
- 65. Thank you
