Ebola - United States - 22 October 2014 - Yale-Tulane Special Report
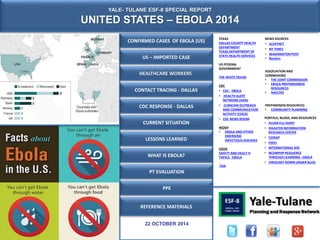
- 1. YALE- TULANE ESF-8 SPECIAL REPORT UNITED STATES – EBOLA 2014 US – IMPORTED CASE HEALTHCARE WORKERS CONTACT TRACING - DALLAS CDC RESPONSE - DALLAS CURRENT SITUATION LESSONS LEARNED WHAT IS EBOLA? PT EVALUATION 22 OCTOBER 2014 TEXAS DALLAS COUNTY HEALTH DEPARTMENT TEXAS DEPARTMENT OF STATE HEALTH SERVICES US FEDERAL GOVERNMENT THE WHITE HOUSE CDC • CDC - EBOLA • HEALTH ALERT NETWORK (HAN) • CLINICIAN OUTREACH AND COMMUNICATION ACTIVITY (COCA) • CDC NEWS ROOM NIOSH • EBOLA AND OTHER EMERGING INFECTIOUS DISEASES OSHA SAFETY AND HEALT H TOPICS - EBOLA FDA REFERENCE MATERIALS NEWS SOURCES • ALERTNET • NY TIMES • WASHINGTON POST • Reuters ASSOCIATION AND COMMISIONS • THE JOINT COMMISSION • EBOLA PREPAREDNESS RESOURCES • NACCHO PREPARENESS RESOURCES: • COMMUNITY PLANNING CONFIRMED CASES OF EBOLA (US) PORTALS, BLOGS, AND RESOURCES • AVIAN FLU DIARY • DISASTER INFORMATION RESEARCH CENTER • CIDRAP • H5N1 • INTERNATIONAL SOS • NCDMPHP RESILIENCE THROUGH LEARNING - EBOLA • VIROLOGY DOWN UNDER BLOG PPE
- 2. CONFIRMED CASES OF EBOLA (US) CASES OF EBOLA OUTSIDE OF WEST AFRICA At least 17 Ebola cases have been treated outside of West Africa in the current outbreak, including two Dallas hospital workers who have tested positive for Ebola. Most of these involve health and aid workers who contracted Ebola in West Africa and were transported back to their home country for treatment. Four cases were diagnosed outside of West Africa: A Liberian man who began showing symptoms four days after arriving in Dallas, a Spanish nurse who became ill after treating a missionary in a Madrid hospital and the two Dallas hospital workers who were involved in the treatment of the Liberian man. These cases are compiled from reports by the federal Centers for Disease Control and Prevention, the World Health Organization, Doctors Without Borders and other official agencies. As of 21 OCT 2014, 3 Ebola patients remain hospitalized in the US. Eight confirmed cases of Ebola have been treated in the United States: 1 died, 6 have been discharged, 2 remain in the hospital. 1 U.S. citizen died abroad, having never returned to the States. • Dr. Kent Brantly (missionary) -- Discharged from Emory University Hospital in Atlanta on August 21. • Nancy Writebol (missionary) -- Discharged from Emory University Hospital on August 19. • Thomas Eric Duncan (Liberian) -- Died October 8; was treated for Ebola at Texas Health Presbyterian Dallas. • Amber Vinson (nurse at Texas Health Presbyterian) -- Currently receiving treatment at Emory University Hospital after being transported from Dallas on October 15. • Nina Pham (nurse at Texas Health Presbyterian) -- Currently receiving treatment; Transferred to a NIH hospital in Maryland, from Dallas, for treatment on October 16, 2014 • Dr. Rick Sacra (missionary) -- Discharged from the Nebraska Medical Center on September 25; was admitted to a hospital in Worcester, Massachusetts, for a respiratory virus on October 4; and was released the following day. • Ashoka Mukpo (NBC News freelancer) – Discharged from the Nebraska Medical on 21 October 2014. • US Doctor (name unknown) -- Discharged from Emory University Hospital after having been hospitalized for 6 weeks. The American doctor who had quietly returned to the U.S. after contracting Ebola working in Sierra Leone in September.
- 3. US – IMPORTED CASE SITUATION: EBOLA IN THE US: A single imported case from Liberia, Thomas Eric Duncan, was confirmed on September 30,2014 with Ebola. Two healthcare workers who tended to Mr Duncan confirmed infected in October, all in Texas. They are the first people to get infected with Ebola within the United States and represent the first person-to-person spread outside of Africa. Extensive contact tracing is currently underway US INDEX PATIENT On September 30, 2014, the Centers for Disease Control and Prevention (CDC) reported that Thomas Eric Duncan traveled from Monrovia, Liberia, on September 19, 2014, and arrived in Dallas, Texas, on September 20. On September 24, he developed symptoms, and sought medical care at 10:00 p.m. on September 25. He was admitted to the hospital on September 28. On September 30, the CDC laboratory confirmed that he was infected with Ebola virus. (CDC- 30 SEP) EXPOSURE IN LIBERIA Thomas Eric Duncan, a Liberian national in his mid-40s, had lived in Monrovia, Liberia. On September 15, 2014, Duncan helped to transfer his housemate and landlord's daughter who had Ebola, to the hospital. The family was turned away due to lack of space and Duncan helped carry Williams from the taxi back into her home, where she died. (NYT-1 OCT) TRAVEL HISORY Duncan flew on September 19 from Monrovia to Brussels, where, according to United Airlines, he took Flight 951 to Washington Dulles Airport and continued to Dallas/Fort Worth on Flight 822, arriving September 20. (NYT-1 OCT) DUNCAN’s TRAVEL HISTORY FROM LIBERIA-WASHINGTON/ DULLES – DALLAS/FT WORTH
- 4. US – IMPORTED CASE DUNCAN IS HOSPITALIZED • The hospital notified Dallas County Health and Human Services (DCHHS) on Monday, September 29, 2014, whose personnel arrived on site shortly thereafter.72 CDC officials were notified later on September 29, but did not arrive at the hospital campus until October 1, 2014. (HEARING - 16 OCT 14) • CDC and Texas Department of State Health Services (DSHS) laboratory testing confirmed the diagnosis of Ebola on Tuesday, September 30, 2014. (HEARING - 16 OCT 14) • DCHHS states it is the lead agency charged with the ongoing contact investigation to determine who may have been exposed to Duncan while he was contagious. The investigation has, thus far, identified forty-eight individuals out of a broader group with risk of exposure. Ten individuals are considered to be at high risk. These forty-eight contacts are being monitored for twenty-one days from their time of exposure. (HEARING - 16 OCT 14) • Duncan received an experimental drug (Brincidofovir)during the course of his treatment. He was also intubated and on dialysis for an unknown period of time. • DEATH: On October 8, 2014, Thomas Eric Duncan dies. (TXDSHS-8 OCT) DEVLOPS SYMPTOMS Duncan began experiencing symptoms on September 24, 2014 and went to the Texas Health Presbyterian Hospital emergency room late in the evening of September 25. During this visit, his reported symptoms were a 100.1 °F (37.8 °C) fever, abdominal pain for two days, a headache, and decreased urination. The ER nurse had asked about his travel history and recorded that he had come from Liberia; however; the significance of this information was missed by the hospital staff. He was diagnosed with a "low-grade, common viral disease" and was sent home with a prescription for antibiotics. (Reuters – 1 OCT) Duncan began vomiting on September 28, 2014, and was transported the same day to Texas Health Presbyterian Hospital emergency room by ambulance where he was diagnosed with Ebola. SOURCE: HEARING ON EXAMINING THE U.S. PUBLIC HEALTH RESPONSE TO THE EBOLA OUTBREAK (16 OCT 14)
- 5. HEALTHCARE WORKERS HOW MANY HEALTH CARE WORKERS HAVE CONTRACTED EBOLA? • The news that a Dallas nurse who helped care for Thomas Eric Duncan was infected with the Ebola virus has fed fears of health care workers across the United States. Nina Pham is the first patient to be infected in the United States. A second nurse treating Duncan, Amber Vinson, has tested positive for Ebola. • More than 400 health care workers in West Africa have been infected with Ebola during the current outbreak, and 233 had died as of Oct. 8. The World Health Organization said that the high rates of infection among medical workers could be attributed to shortages or improper use of protective equipment; not enough medical personnel; and long working hours in isolation wards. TWO US HEALTHCARE WORKERS CONTRACT EBOLA • 11 OCT - A healthcare worker, Nina Pham, 26, a nurse who cared for Duncan at Texas Presbyterian Hospital, reported having a low grade fever overnight and was referred for testing. The Texas Department of State Health Services’ laboratory returned a preliminary test that was positive for Ebola at approximately 9:30 p.m. on October 11. (16 OCT 14) • 12 OCT - CDC testing performed on October 12 confirmed this result. Pham is isolated and interviewed by CDC to identify any contacts or potential community exposures. To date, CDC officials have identified one close contact, who is being monitored for fever and other symptoms. (16 OCT 14) • 13 OCT - Amber Vinson, 29, another nurse who treated Duncan at Texas Health Presbyterian Hospital flies from Cleveland to Dallas on Frontier Airlines Flight 1143, arriving at 8:16 p.m. She has no symptoms, but her temperature was 99.5 degrees that morning. She called the Centers for Disease Control and Prevention before boarding, and no one told her not to fly. (ABC NEWS - 16 OCT) • 14 OCT - Vinson is taken to Texas Health Presbyterian Hospital in Dallas with a fever. (ABC NEWS - 16 OCT) • 15 OCT - Vinson is diagnosed with Ebola shortly after midnight and flown to Emory University Hospital that evening .( TXDSHA – 15 OCT) • 16 OCT - Nina Pham, the first person to contract Ebola in the United States while caring for a patient in Dallas, was transferred to a National Institutes of Health Clinical Center in Bethesda. Pham's transfer to the facility, one of four in the United States with a special biocontainment unit, occurred Thursday evening, October 16, 2014. (WP- 16 OCT)
- 6. CONTACT TRACING - DALLAS INITIAL CONTACT TRACING - DUNCAN • Authorities began tracing Duncan’s contacts and initially began monitoring around 100 people who may have had contact with the Ebola patient. This conservative approach cast a 'wide net' and includes people who are likely not at risk but were screened anyway. (CDC- 10 OCT) • During the CDC's press briefing., it was confirmed that 10 people had contact with the Duncan, none of whom had symptoms, and the rest had possible contact. (CDC- 10 OCT) • Four close family members of the patient, believed to be amongst the “high risk” contacts, were asked to stay home at least until October 19, when the 21-day incubation period for the virus would have lapsed. After failing to comply with this request, they were formally ordered to remain confined to their apartment. The family was forced to remain in the apartment for days, despite the fact that it was contaminated with Duncan’s waste products and bodily fluids. The family has since been moved to an undisclosed location. (HEARING - 16 OCT 14) INITIAL CONTACT TRACING – PHAM: According CDC there is only one person who may have had contact with Nina Pham while she had symptoms/could possibly have spread Ebola to others. That person is under "active monitoring" and has no symptoms. (SOS – 12 OCT) INITIAL CONTACT TRACING – VINSON: Amber Vinson’s contacts tracing is more complex due to her travel. CDC and Frontier Airlines are tracking those who were on her flights .(CDC- 15 OCT)
- 7. CONTACT TRACING - DALLAS Public health officials attempt to reach all contacts/possible contacts every day to check for fever and other symptoms. Daily follow-up with contacts/possible contacts will continue for 21 days from the date of each person’s exposure. (CDC- 16 OCT) CDC EXPANDS PASSENGER NOTIFICATION Based on additional information obtained during interviews of close contacts to the second healthcare worker from Texas Presbyterian Hospital who tested positive for Ebola, the Centers for Disease Control and Prevention (CDC) is expanding its outreach to airline passengers who flew from Dallas Fort Worth to Cleveland on Frontier flight 1142 on Oct. 10. CDC is now asking passengers on Frontier Airlines flight 1142 Dallas/Fort Worth to Cleveland on Oct. 10 and passengers on Frontier Airlines flight 1143 from Cleveland to Dallas/Fort Worth on Oct. 13 to call 1 800-CDC INFO (1 800 232-4636). Public health professionals will interview passengers about the flight, answer their questions, and arrange follow up if warranted. Individuals who are determined to be at any potential risk will be actively monitored. (CDC - 16 OCT) DATE: 10/17/2014 - Numbers are accurate as of 5 p.m., 16 OCT are updated at approximately noon each day. CONFIRMED CASES: 3 * CONTACTS: 11 **POSSIBLE CONTACTS: 132 TOTAL: 143 * Contacts – Definite exposure ** Possible Contacts – Possible exposure NOTE: The number of possible contacts increased significantly Oct. 14 to account for a group of healthcare workers who were previously self-monitoring and are now being actively monitored following a healthcare worker's Ebola diagnosis over the weekend. Another case was diagnosed Oct. 15, which also impacted the numbers. Contacts are defined as people who had definite exposure to an Ebola patient.
- 8. CDC RESPONSE - DALLAS CDC SUPPORT IN DALLAS • In addition to an initial team of 10 public health professionals sent on September 30 to support contact tracing and response after an index patient was hospitalized with Ebola in Dallas, CDC has sent new resources to Dallas to support the highest standard of infection control. (14 OCT) • CDC has deployed a second team of 16 to Dallas to train and assist the hospital in infection control and the monitoring of health care workers who had contact with the index patient. • These join the 2 CDC officials who were assisting the hospital previously. The additional CDC team includes experts in: ‒ Infection control ‒ Ebola virus control and infectious diseases ‒ Laboratory science ‒ Personal protective equipment ‒ Hospital epidemiology ‒ Workplace safety • The team includes experts who successfully controlled outbreaks of Ebola in Africa in the past two decades, including in health-care settings. Team members have worked with Doctors Without Borders on infection control protocols and trained others in Africa to follow those protocols. • In addition, two infection control nurses from Emory University hospital who successfully treated Ebola patients without contracting or transmitting infection joined the response at the Dallas hospital to provide peer-to-peer training and support. FOCUS OF THE DALLAS HOSPITAL INVESTIGATION The CDC team is assisting the hospital in rapidly reducing the risk of further spread of Ebola and investigating how the healthcare workers may have become infected with Ebola. The team is evaluating: • What personal protective equipment (PPE) is being used and how it is being put on and taken off ? • What medical procedures were done on the index patient that may have exposed the healthcare worker? • The decontamination processes for workers leaving the isolation unit ? • Oversight and monitoring of all infection control practices, particularly putting on and taking off PPE, at each shift in each location where this occurs? • What enhanced training and/or changes in protocol may be needed? FOR MORE DETAILS SEE: http://www.cdc.gov/media/releases/2014/fs1014-ebola-investigation- fact-sheet.pdf
- 9. CURRENT SITUATION The President has put into motion the following action to ensure we effectively treat and prevent the spread of Ebola (15 OCT): • The CDC will now send a rapid response team, a "swat team, essentially" to be on the ground within 24 hours as soon as someone is diagnosed with Ebola so the CDC can walk the local hospital through the protocols step-by-step. That includes use and disposal of protective equipment. • Lessons learned from the problems that occurred in Dallas to hospitals, clinics, and first-responders will be communicated around the country on a ongoing and up-to-date basis. • The federal government will work carefully with the city of Dallas and the state of Texas to ensure that, in the event any other cases arise among health workers, they are properly cared for in a way that is consistent with public safety. • Continue to conduct “contact-tracing" to ensure that anyone who may have come into contact with the affected individuals are being monitored in a way to prevent the further spread of this disease. • Continue to monitor the health status of the other health care workers in Dallas. • Continue screening processes at airports and make sure teams are in place to transport suspected cases to specialized, secure hospitals if needed. • Continue to lead the international response in West Africa because "the investment we make in helping Liberia, Sierra Leone, and Guinea deal with this problem is an investment in our own public health." President Obama has asked Ron Klain, who served as chief of staff to both Vice President Biden and former vice president Al Gore, to manage the government’s response to the deadly virus as public anxiety grows over its possible spread. (WP-17 OCT). The United States issued stringent new protocols on Monday, October 20,2014 for health workers treating Ebola victims, directing medical teams to wear protective gear that leaves no skin or hair exposed to prevent medical workers from becoming infected. Under new protocols, Ebola healthcare workers also must undergo special training and demonstrate competency in using protective equipment. Use of the gear, now including coveralls, and single-use, disposable hoods, must be overseen by a supervisor to ensure proper procedures are followed when caring for patients with Ebola, which is transmitted through direct contact with bodily fluids but is not airborne. (CDC protocols: (CDC-20 OCT)) The Pentagon will create a 30-person team of medical experts that will provide support for civilian doctors who might lack proficiency in the deadly Ebola virus or other infectious diseases. (WP-19 OCT) The Pentagon announced Sunday that it will create a 30-person team of medical experts that could quickly leap into a region if new Ebola cases emerge in the United States, providing support for civilian doctors who lack proficiency in fighting the deadly virus. Defense Secretary Chuck Hagel ordered the Pentagon’s Northern Command, which has a prime focus on protecting homeland security, to send this new team to Fort Sam Houston in Texas for high-level preparations to respond to any additional Ebola cases beyond the three confirmed in the country.
- 10. CURRENT SITUATION - TRAVEL TEXAS HEALTH OFFICIALS ORDER ANY PERSON WHO ENTERED THE ROOM OF THE FIRST EBOLA PATIENT AT A DALLAS HOSPITAL NOT TO TRAVEL BY PUBLIC TRANSPORT Texas health officials have instructed any person who entered the room of the first Ebola patient at a Dallas hospital not to travel by public transport, including planes ship, buses or trains, or visit groceries, restaurants or theaters for 21 days, until the danger of developing Ebola has expired. (17 OCT) The instructions, issued by the Texas Department of State Health Service late Thursday, cover more than 70 health workers involved in providing care for Thomas Duncan, the Liberian national who became the first patient to test positive for Ebola in the United States. Amber Vinson, 29, a nurse who treated Duncan and became ill with Ebola traveled on Frontier Airlines from Dallas to Cleveland and back THE DEPARTMENT OF HOMELAND SECURITY ANNOUNCED IT WOULD BEGIN REQUIRING ALL PASSENGERS FROM THREE WEST AFRICAN COUNTRIES AFFECTED BY EBOLA (LIBERIA, SIERRA LEONE OR GUINEA) TO ARRIVE ONLY AT THE FIVE U.S. AIRPORTS WITH HEIGHTENED SECURITY MEASURES. • The five airports are John F. Kennedy International in New York, O’Hare International in Chicago, Hartsfield-Jackson International in Atlanta, Washington Dulles International near Washington, D.C., and Newark Liberty International in Newark, N.J. • Thee new measures would go into effect on Wednesday, September 22 (WSJ- 21 OCT) • There are no direct flights from the three countries to the U.S. • Just three big international airlines serve Liberia, Guinea and Sierra Leone: Air France-KLM SA, Brussels Airlines and Royal Air Maroc of Morocco. Most travelers from those countries connect to the U.S. via Paris, Brussels or Casablanca, Morocco. • The CDC and the Department of Homeland Security (DHS) announced that the following five U.S. airports will begin enhanced Ebola screening for all travelers coming from Ebola-affected countries: John F. Kennedy International Airport (in New York), Newark, Washington-Dulles, Chicago O'Hare and Atlanta. (WHITE HOUSE – 8 OCT) . • Screening was initiated at JFK on 11 OCT (WSJ- 11 OCT), and at Atlanta, Chicago, Washington, Newark airports on 16 OCT (AP -16 OCT)
- 11. PRELIMINARY LESSON LEARNED FROM DALLAS DIAGNOSING EBOLA IS VERY DIFFERENT FROM TREATING EBOLA Texas Health Presbyterian Hospital Dallas (THD) was and remains well prepared and equipped based upon the best available information to treat patients already identified as having EVD. Where THD fell short initially was in its ability to detect and diagnose EVD, as evidenced by Mr. Duncan’s first visit to the ED. As a result, following Mr. Duncan’s initial admission, THD have changed their screening process in the ED to capture the patient’s travel history at the first point of contact with ED staff. This process change makes the travel history available to all caregivers from the beginning of the patient’s visit in the ED. Additionally, THD have modified its Electronic Health Record (HER) in multiple ways to increase the visibility and documentation of information related to travel history and infectious exposures related to EVD. These include: • Better placement/title of the screening tool • Expanded screening questions, which include: – Exposure to persons known or suspected to have EVD – High-risk activities for persons who have traveled to Ebola endemic areas such as: “have you touched a dead animal or helped carry someone sick” – A pop up identifying the patient as high-risk for Ebola with explicit instructions for next steps if the answer to any of the screening questions is positive COMMUNICATION IS CRITICAL BUT IT IS NO SUBSTITUTE FOR TRAINING Despite the communications regarding EVD preparedness that occurred between August 1 and October 1, THD realized a need for more proactive, intensive, and focused training for frontline responders in the diagnosis of EVD. Therefore an E) refresher course was provided to THD ED nurses. Additionally, an “in -service” face-to-face training was provided starting with the night shift and continued at the start of every shift for a number of days. The education included screening of suspected patients, documenting response to travel questions in the Electronic Health Record and proper donning and offing of PPE EBOLA EXTENDS BEYOND THE WALLS OF THE HOSPITAL In a crisis like this, a hospital’s focus needs to be on providing exceptional care. Coordination and collaboration with federal, state, and local agencies is critical to limiting the perimeter of Ebola, managing contact identification interviews, and establishing community confidence. SOURCE: DR. DANIEL VARGA, CHIEF CLINICAL OFFICER AND SENIOR VICE PRESIDENT, TEXAS HEALTH RESOURCES (16 OCT 2014)
- 12. PRELIMINARY LESSON LEARNED FROM DALLAS HEALTHCARE WORKERS WHO ARE EXPOSED SHOULD NOT TRAVEL Amber Vinson, the second health care worker, had a fever of 99.5 degrees when she flew from Cleveland to Dallas, according to the CDC. While other passengers' risks of exposure are low, the fact that she was being monitored due to exposure and had a slight fever meant that she definitely should not have been on a plane. LESSON LEARNED: CDC guidance in this setting outlines the need for what is called “ controlled movement”. That can include a charter plane, a car, but it does not include public transport. CDC will from this moment forward ensure that no other individual who is being monitored for exposure undergoes travel in any way other than controlled movement. (CDC – 15 OCT ) HOSPITAL PREPAREDNESS Both infected healthcare workers have been evacuated to specialized hospitals that have biocontainment units and highly trained staff in infectious diseases. The problem is that not all hospitals are equally prepared or equipped to combat Ebola. There are four hospitals in the country that have top-level biocontainment units including the Emory University Hospital in Atlanta and NIH Medical Center in Bethesda, Maryland, University of Nebraska in Omaha and St. Patrick Hospital in Missoula, Montana. There are limited beds available at these facilities (approx. 12 beds in total). Using these hospitals alone is only feasible as long as the number of cases in the US remain low. LESSON LEARNED: • DIAGNOSIS: Every hospital in the country needs to be ready to diagnose Ebola . • PERSONAL PROTECTIVE EQUIPMENT ‒ PPE suits will be standardized, to include a specific type of suit to ensure consistency in both training and use, possibly using only full-body suits. This is consistent with current CDC recommendations. ‒ Use of a model of hood that protects health care worker’s neck to prevent exposure. ‒ Removing PPE now includes an enhanced and detailed step-by-step disinfection of hands process with specific sequencing for removal of each piece of equipment and the hand washing required. • OVERSIGHT AND MONITORING: The single most important aspect of safe care of Ebola is to have a site manager at all times who oversees the putting on and taking off of PPE and the care given in the isolation unit. A site manager is now in place and will be at the hospital 24/7 as long as Ebola patients are receiving care • ESTABLISH A DEDICATED CDC RESPONSE TEAM: CDC is setting up a dedicated CDC Response Team that could be on the ground at any hospital that receives a confirmed Ebola infected patient within a few hours. The CDC Response Team would provide in person, expert support and training on infection control, healthcare safety, medical treatment contact tracing, waste and decontamination, public education and other issues. The CDC Response Team would help ensure that clinician, and state and local public health practitioners consistently follow strict standards of protocol to ensure safety of the patient and healthcare workers
- 13. WHAT IS EBOLA? Starts with: • Sudden onset of fever (greater than 38.6°C or 101.5°F) • Intense weakness, muscle pain • Headache, sore throat Followed by: • Vomiting, diarrhea, rash • Impaired kidney and liver function • Internal and external bleeding Ebola creates holes in blood vessels, often causing bleeding and shock. It does this by killing endothelial cells, which form the blood vessels’ lining and other partitions in the body. When those cells die, blood and other fluids can leak out. Organs shut down. The virus replicates very quickly, before most people’s bodies can mount an attack. People often have massive bleeding 7 to 10 days after infection. It effectively disables the immune system by hampering the development of antibodies and T cells that would target the virus. Scientists are not certain exactly how. (Washington Post) WHAT IS EBOLA? • Ebola virus disease (EVD), formerly known as Ebola hemorrhagic fever, is a severe, often fatal illness in humans, caused by a filovirus. • EVD outbreaks have a case fatality rate of up to 90%. • First appeared in 1976 in Sudan and Democratic Republic of Congo. The latter was in a village situated near the Ebola River, from which the disease takes its name. HOW IS IT TRANSMITTED SIGNS AND SYMPTOMS • The virus that causes Ebola is not airborne • Ebola is spread by close contact with an infected person. • Ebola is spread through direct contact with: o Blood or body fluids (such as saliva, sweat, vomit, semen, stool or urine) of an infected person or animal, or o Through contact with objects that have been contaminated with the blood or other body fluids of an infected person. RISK OF EXPOSURE • Healthcare providers caring for Ebola patients and the family and friends in close contact with Ebola patients are at the highest risk of contracting Ebola because they may come in contact with the blood or body fluids of sick patients. • People also can become infected with Ebola after coming in contact with infected wildlife. For example, in Africa, Ebola may be spread as a result of handling bush meat (wild animals hunted for food) and contact with infected bats. WAYS IN WHICH THE VIRUS IS TRANSMITTED. SOURCE: THE HERALD SOURCE : CDC WHO KEY POINTS – EBOLA VIRUS DISEASE, WEST AFRICA INCUBATION: The incubation period is usually four to ten days but can vary from two to 21 days (most commonly 8-10 days)
- 14. DIAGNOSIS WHAT IS EBOLA? • Early diagnoses difficult because symptoms are nonspecific to Ebola • Definitive diagnoses made through laboratory testing: ‐ PCR ‐ ELISA ‐ Virus isolation ‐ IgM and IgG antibodies TREATMENT • Symptoms of Ebola are treated as they appear. The following basic interventions, when PREVENTION • Avoid all contact with blood or fluids of infected people • Isolation of Ebola patients • Basic infection control measures ‐ Equipment sterilization ‐ Routine disinfection ‐ Hand hygiene • Prompt and safe burial of dead SOURCE : CDC WHO used early, can significantly improve the chances of survival: • Providing intravenous fluids (IV)and balancing electrolytes (body salts) • Maintaining oxygen status and blood pressure • Treating other infections if they occur • No FDA-approved vaccine or medicine (e.g., antiviral drug) is available for Ebola. • Experimental vaccines and treatments for Ebola are under development, but they have not yet been fully tested for safety or effectiveness. • Recovery from Ebola depends on good supportive care and the patient’s immune response. People who recover from Ebola infection develop antibodies that last for at least 10 years, possibly longer. It isn't known if people who recover are immune for life or if they can become infected with a different species of Ebola. Some people who have recovered from Ebola have developed long-term complications, such as joint and vision problems.
- 15. PATIENT EVALUATION 1. Activate the hospital preparedness plan for Ebola, which should include • Initiate the notification plan for suspect or confirmed Ebola patient immediately. • Ensure hospital infection control is notified. • Create a clinical care team led by a senior level experienced clinician that includes at a minimum a hospital infection control specialist, a senior nurse, an infectious disease specialist, and critical care consultants. • Assign a senior staff member from the clinical care team to coordinate testing and reporting of results from the hospital laboratory, state health department laboratory, CDC, and local and state public health. For a list of state and local health department phone numbers, see http://www.cdc.gov/vhf/ebola/outbreaks/state-local-health-department-contacts. html. 2. Isolate the patient in a separate room with a private bathroom. 3.Ensure a standardized protocol is in place for how and where to remove and dispose of personal protective equipment (PPE) properly and that this information is posted in the patient care area. 4.When interviewing the patient, collect data on: • Earliest date of symptom onset and the sequence of sign/symptom development preceding presentation to an emergency department. • Detailed and precise travel history (e.g., dates, times, locations). • Names of any persons with whom the patient may have had contact during and any time after the earliest date of symptom onset. 5. Consider and evaluate for all potential alternative diagnoses (e.g. malaria, typhoid fever). 6. Ensure patient has the ability to communicate with family. GENERAL INFORMATION Ebola virus disease Information for Clinicians in U.S. Healthcare Settings Safe Management of Patients with Ebola Virus Disease (EVD) in U.S. Hospitals Could It Be Ebola Poster
- 16. EBOLA PREPAREDNESS CONSIDERATIONS FOR OUTPATIENT/AMBULATORY CARE SETTINGS Go to http://www.phe.gov/Preparedness/responders/ebola/Documents/ebola-preparedness-considerations.pdf to download this document with its active hyperlinks
- 17. GUIDANCE ON PERSONAL PROTECTIVE EQUIPMENT TO BE USED BY HCW DURING MANAGEMENT OF PATIENTS WITH EBOLA VIRUS DISEASE IN U.S. HOSPITALS KEY PRINCIPLES: • Prior to working with Ebola patients, all healthcare workers involved in the care of Ebola patients must have received repeated training and have demonstrated competency in performing all Ebola-related infection control practices and procedures, and specifically in donning/doffing proper PPE. • While working in PPE, healthcare workers caring for Ebola patients should have no skin exposed. • The overall safe care of Ebola patients in a facility must be overseen by an onsite manager at all times, and each step of every PPE donning/doffing procedure must be supervised by a trained observer to ensure proper completion of established PPE protocols. DURING PATIENT CARE • PPE must remain in place and be worn correctly for the duration of exposure to potentially contaminated areas. PPE should not be adjusted during patient care. • Healthcare workers should perform frequent disinfection of gloved hands using an ABHR, particularly after handling body fluids. • If during patient care a partial or total breach in PPE (e.g., gloves separate from sleeves leaving exposed skin, a tear develops in an outer glove, a needlestick) occurs, the healthcare worker must move immediately to the doffing area to assess the exposure. Implement the facility exposure plan, if indicated by assessment. DOFFING • The removal of used PPE is a high-risk process that requires a structured procedure, a trained observer, and a designated area for removal to ensure protection • PPE must be removed slowly and deliberately in the correct sequence to reduce the possibility of self-contamination or other exposure to Ebola virus • A stepwise process should be developed and used during training and daily practice PRINCIPLES OF PPE: Healthcare workers must understand the following basic principles to ensure safe and effective PPE use, which include that no skin may be exposed while working in PPE: DONNING • PPE must be donned correctly in proper order before entry into the patient care area and not be later modified while in the patient care area. • The donning activities must be directly observed by a trained observer. GO TO http://www.cdc.gov/vhf/ebola/hcp/procedures-for-ppe.html for the guidance on PPE that CDC put out as of 20 OCT 2014
- 18. GUIDANCE ON PERSONAL PROTECTIVE EQUIPMENT TO BE USED BY HCW DURING MANAGEMENT OF PATIENTS WITH EBOLA VIRUS DISEASE IN U.S. HOSPITALS DOUBLE GLOVING • Double gloving provides an extra layer of safety during direct patient care and during the PPE removal process. • Beyond this, more layers of PPE may make it more difficult to perform patient care duties and put healthcare workers at greater risk for percutaneous injury (e.g., needlesticks), self-contamination during care or doffing, or other exposures to Ebola. • If healthcare facilities decide to add additional PPE or modify this PPE guidance, they must consider the risk/benefit of any modification, and train healthcare workers on correct donning and doffing in the modified procedures. TRAINING ON CORRECT USE OF PPE • Training ensures that healthcare workers are knowledgeable and proficient in the donning and doffing of PPE prior to engaging in management of an Ebola patient. • Comfort and proficiency when donning and doffing are only achieved through repeated practice on the correct use of PPE. Healthcare workers should be required to demonstrate competency in the use of PPE, including donning and doffing while being observed by a trained observer, before working with Ebola patients. • In addition, during practice, healthcare workers and their trainers should assess their proficiency and comfort with performing required duties while wearing PPE. Training should be available in formats accessible to individuals with disabilities or limited English proficiency. Target training to the educational level of the intended audience. USE OF A TRAINED OBSERVER • Because the sequence and actions involved in each donning and doffing step are critical to avoiding exposure, a trained observer will read aloud to the healthcare worker each step in the procedure checklist and visually confirm and document that the step has been completed correctly. • The trained observer is a dedicated individual with the sole responsibility of ensuring adherence to the entire donning and doffing process. • The trained observer will be knowledgeable about all PPE recommended in the facility’s protocol and the correct donning and doffing procedures, including disposal of used PPE, and will be qualified to provide guidance and technique recommendations to the healthcare worker. • The trained observer will monitor and document successful donning and doffing procedures, providing immediate corrective instruction if the healthcare worker is not following the recommended steps. The trained observer should know the exposure management plan in the event of an unintentional break in procedure. CDC recommends facilities use a powered air-purifying respirator (PAPR) or an N95 or higher respirator in the event of an unexpected aerosol-generating procedure. SOURCE: CDC - 20 OCT
- 19. GUIDANCE ON PERSONAL PROTECTIVE EQUIPMENT TO BE USED BY HCW DURING MANAGEMENT OF PATIENTS WITH EBOLA VIRUS DISEASE IN U.S. HOSPITALS Given the intensive and invasive care that U.S. hospitals provide for Ebola patients, the tightened guidelines are more directive in recommending no skin exposure when PPE is worn. CDC is recommending all of the same PPE included in the August 1, 2014 guidance, with the addition of coveralls and single-use, disposable hoods. Goggles are no longer recommended as they may not provide complete skin coverage in comparison to a single-use, disposable full-face shield. Additionally, goggles are not disposable, may fog after extended use, and healthcare workers may be tempted to manipulate them with contaminated gloved hands. PPE RECOMMENDED FOR U.S. HEALTHCARE WORKERS CARING FOR PATIENTS WITH EBOLA INCLUDES: • Double gloves • Boot covers that are waterproof and go to at least mid-calf or leg covers • Single-use fluid resistant or impermeable gown that extends to at least mid-calf or coverall without integrated hood. • Respirators, including either N95 respirators or powered air purifying respirator (PAPR) • Single-use, full-face shield that is disposable • Surgical hoods to ensure complete coverage of the head and neck • Apron that is waterproof and covers the torso to the level of the mid-calf (and that covers the top of the boots or boot covers) should be used if Ebola patients have vomiting or diarrhea The guidance describes different options for combining PPE to allow a facility to select PPE for their protocols based on availability, healthcare personnel familiarity, comfort and preference while continuing to provide a standardized, high level of protection for healthcare personnel. The guidance includes having: SOURCE: CDC - 20 OCT PHOTOS: University of Nebraska Medical Center (UNMC)
- 20. DONNING BIOLOGICAL PPE- EBOLA PATIENTS (UNIVERSITY OF NEBRASKA) http://app1.unmc.edu/nursing/heroes/pdf/vhfppe/donningBiologicalPPE-EbolaPatients-8.5x11-CC-v1.02.pdf
- 21. DONNING BIOLOGICAL PPE- EBOLA PATIENTS (UNIVERSITY OF NEBRASKA) http://app1.unmc.edu/nursing/heroes/pdf/vhfppe/donningBiologicalPPE-EbolaPatients-8.5x11-CC-v1.02.pdf
- 22. DOFFING BIOLOGICAL PPE- EBOLA PATIENTS (UNIVERSITY OF NEBRASKA) http://app1.unmc.edu/nursing/heroes/pdf/vhfppe/doffingBiologicalPPE-EbolaPatients-8.5x11-CC-v1.01.pdf
- 23. DOFFING BIOLOGICAL PPE- EBOLA PATIENTS (UNIVERSITY OF NEBRASKA) http://app1.unmc.edu/nursing/heroes/pdf/vhfppe/doffingBiologicalPPE-EbolaPatients-8.5x11-CC-v1.01.pdf
- 24. DOFFING BIOLOGICAL PPE- EBOLA PATIENTS (UNIVERSITY OF NEBRASKA) http://app1.unmc.edu/nursing/heroes/pdf/vhfppe/doffingBiologicalPPE-EbolaPatients-8.5x11-CC-v1.01.pdf
- 25. REFERENCE DIAGNOSIS • Case Definition for Ebola Virus Disease (EVD) SPECIMEN COLLECTIONS • Interim Guidance for Specimen Collection, Transport, Testing, and Submission for Persons Under Investigation for Ebola Virus Disease in the United States • Factsheet: Interim Guidance for Specimen Collection, Transport, Testing, and Submission for Patients with Suspected Infection with Ebola Virus Disease[PDF - 1 page] MONITORING AND MOVEMENT • Interim Guidance for Monitoring and Movement of Persons with Ebola Virus Disease Exposure PT TRANSPORT • Guidance: Air Medical Transport for Patients with Ebola • Interim Guidance: EMS Systems & 9-1-1 PSAPs: Management of Patients in the U.S. PATIENT MANAGEMENT • Safe Management of Patients with Ebola Virus Disease (EVD) in U.S. Hospitals INFECTION CONTROL • Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals • Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus HANDLING OF REMAINS • Guidance for Safe Handling of Human Remains of Ebola Patients in U. S. Hospitals and Mortuaries
