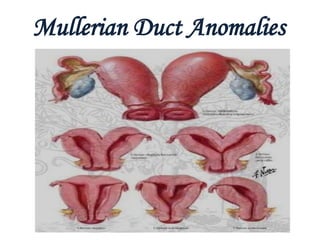
Mullerian anomalies
- 2. MULLERIAN DUCTS Paired ducts derived from intermediate mesoderm. Known as paramesonephric duct. Named after Johannes peter mullero-described them in 1830.
- 3. EMBRYOLOGICAL DEVELOPMENT Appear between 5-6 wks. Derived from intermediate mesoderm lateral to wolffian duct as invagination of dorsal coelomic epithelium. Depends on absence of male determining factor which is present in Y-chromosome.
- 4. Cont. Female development called Basic developmental path of the human embryo – requires not estrogen but the absence of testosterone. Ambisexual period persist upto 8 wks, thereafter one type of duct system persist & other disappears.
- 5. Development of Genital Ducts • Both male and female embryos have two pairs of genital ducts • The mesonephric ducts (wolffian ducts) play an important role in the development of the male reproductive system • The paramesonephric ducts (mullerian ducts) have a leading role in the development of the female reproductive system • Till the end of sixth week, the genital system is in an indifferent state, when both pairs of genital ducts are present
- 7. Cont. Mullerian ducts form as buds of coelomic epithelium . Grows downward & lateral to corresponding wolffian ducts. Turn inwards & crosses anterior to it joining its fellow from opposite side.
- 8. Consists of- Upper vertical part lateral to wolffian duct → fallopian tube. Middle horizontal part crossing wolffian duct → remaining part of fallopian tube. Lower vertical part fusing to opposite part → uterus, cervix, upper 1/3rd of vagina. In forming the uterus, the mullerian ducts fuses from below upwards
- 9. Cont. VAGINA Develops in 3rd month of embryonic life. From lower end of uterovaginal canal (mullarian duct) & urogenital sinus. Uterovaginal canal fuses with sinovaginal bulb (develops from posterior aspect of urogenital sinus)forming vaginal plate. Later canalizes to form vaginal canal.
- 11. Cont. Upper 1/3rd develops from mullerian duct – mesodermal. Lower 2/3rd develops from vaginal plate – endodermal. Incomplete breakdown of the junction between the bulbs and the urogenital sinus proper leaves the hymeneal membrane. .
- 12. The Development of the Gonads The phase of indifferent gonads (Genital Ridge): The germ cells (primordial germ cells) migrate to the genital ridge by the 6th week. The germ cells influence development of the gonad into ovary or testes The covering epithelium proliferates and sends cluster of cells into the underlying mesoderm known as the cells of the sex cords. Differentiate into testis or ovaries depending on the presence or absence of the Y chromosome in the germ cells. Ovarian Differentiation Occur in the the absence of Y chromosome and SRY protein it occurs two weeks later (about the 8th week)
- 13. The cortical zone that contain the germ cells develop to a much greater extent, while the medulla regress. By the fourth month: each germ cell, now become known as Oogonia, is surrounded by a single layer of epithelial cells The oogonia are transformed into primary oocytes as they enter the 1st meiotic division and arrest in prophase until puberty and beginning of ovulation. Around the 20th week of gestation the ovary contains about 7 million germ cells. Degeneration and atresia begins around 20 weeks and by birth approximately 20 million germ cells remain.
- 15. Three main principles governs the practical approach to mullerian anomalies. 1. Mullerian and wolffian ducts are so closely related embryologically that mullerian anomalies are commonly associated with anomalies of kidney and ureter. 2. Development of gonads is separate from ducts so normal ovaries are present in mullerian anomalies. 3. Mullerian anomalies may be associated with anomalies in sex chromosome make up of individual.
- 16. Complete formation & differentiation of mullerian duct into female reproductive system depends on completion of 3 phases of development as follows- □ Organogenesis □ Fusion □ Septal resorption
- 17. ORGANOGENESIS One or both mullerian duct may not develop fully-Uterine agenesis or hypoplasia Unicornuate uterus. FUSION Lateral fusion- process during which lower segment of paired mullerian duct fuse – Uterine didelphys or Bicornuate uterus,Arcuate uterus.
- 18. Cont. Vertical fusion- Fusion of ascending sinovaginal bulb with descending mullerian duct – Transverse vaginal septum, Imperforate hymen. SEPTAL RESORPTION – after fusion central septum persist later resorps to form single uterocervical cavity – Septate uterus
- 19. INCIDENCE There are irregularities in incidence & prevalence rate because of – – Non standardization of classification system. – Non-uniform diagnostic modalities. – Different study population.
- 20. Cont. Normal / Fertile women-1.5-4.5% Infertile patients – 3-6% Women with recurrent miscarriage - 5-10% DISTRIBUTION Septate uterus- 35% Bicornuate-26% Arcuate uterus-18% Unicornuate uterus-10% Didelphys uterus-8%
- 21. Clinical Presentation Uterine anomalies are often an incidental diagnosis while seeing the patient for a different complaint. The Patient can present with: Pelvic pain (cyclic or non-cyclic) Dysmenorrhea Abnormal vaginal bleeding Vaginal pain Uterine rupture during pregnancy Recurrent pregnancy loss Patient may have a concurrent renal abnormalities
- 22. DIAGNOSIS Physical examination Gynecologic Ultrasonography Pelvic MRI Hysterosalpinography Laparoscopy and/or Hysteroscopy may be indicated.
- 24. HYSTEROSALPINGOGRAM- Primary imaging modality. Normal uterus- typical trigone, configuration. Diagnostic criteria. Intercornual distance • Distance between the distal ends of horns. • Septate uterus- <2 cm. • Didelphys uterus- >4 cm. • Normal uterus (indeterminate in an abnormal cavity)- 2-4 cm
- 25. Cont. Intercornual angle • Angle formed by the most medial aspect of two uterine hemicavities. • Septate uterus- <60º Bicornuate uterus- >105º T- shaped uterus • A hypoplastic, irregular, T shaped uterine cavity – inutero DES exposure. • Only anomaly in which HSG plays a significant role- DES exposure.
- 26. Cont. Allows misdiagnosis between- Partial septate & bicornuate uterus. Complete septate & Uterus didelphys.
- 27. ULTRASONOGRAPHY Most commonly 2D is used to evaluate. ( 75-100% sensitivity, upto 90% specificity). Diagnose associated urological anomaly. I Hypoplasia/Agenesis • Absence of uterus & cervix- Agenesis. • Hypoplastic uterus <2 cm intercornual distance- Hypoplasia.
- 28. Cont. Unicornuate uterus- • Difficult to differantiate from normal. • Banana shaped uterus. • Laterally positioned. • Rudimentary horn- soft tissue mass with echogenicity similar to myometrium. • Obstructed horn with functioning endometrium-complex hemorrhagic cyst.
- 29. Cont. Uterus didelphys- • Two separate uterus with two cervix, separate vagina difficult to see. • Endometrial & myometrial zonal width are preserved. Bicornuate uterus- • Two uterine cavity with normal endometrium. • Reliable means of distinguisihing bicornuate from septate uterus.
- 30. Cont. • Concave fundus with fundal cleft >1 cm. • Increased intercornual distance>4 cm. • Intervening septum echogenicity similar to myometrium. Septate uterus • Convex fundal contour. • Intercornual distance <2 cm. • Intervening septum composed of muscle or fibrous tissue.
- 31. Cont. Arcuate uterus • May be detected. • Fundal cleft <1 cm. • Clinically not significant. DES related • Uterine hypoplasia. • Diagnosed confidently by HSG.
- 32. 3 D ULTRASONOGRAPHY Permits accurate diagnosis. Sensitivity & specficity-98.4%,100% resp. It is best performed during the secretory phase of the menstrual cycle so the endometrial cavity is easier to outline. The coronal plane is the most valuable in the detection of uterine anomalies, shows the entire endometrial canal & its relation to myometrium and the uterine serosa. Multiple planes can be constructed regardless of uterine position.
- 33. Cont. Accurately analyses uterine structure, contour of fundus, muscular thickness, septum length.
- 34. MAGNETIC RESONANCE IMAGING Gold standard for diagnosing uterine anomaly. Evaluate concomitant urinary tract anomaly. Hypoplasia/agenesis • Absence of uterus, cervix & upper vagina. • Hypoplastic uterus - <2 cm intercornual distance- Hypoplasia. • Zonal differentiation is poor.
- 35. Cont. Unicoruate uterus- • Banana or cigar shaped uterine cavity. • Laterally deviated. • Preserved zonal anatomy. • Rudimentary horn- soft tissue mass with intensity similar to myometrium. • Obstructed horn with functioning endometrium-distended with blood or blood products.
- 36. Cont. Uterus didelphys • Two separated uterus & cervix. • Preserved zonal anatomy. • Septum of low signal intensity seen within the upper vagina. Bicornuate uterus • Two uterine cavity with single cervix. • Preserved zonal anatomy.
- 37. Cont. • Concave fundus with fundal cleft >1 cm. • Increased intercornual distance>4 cm. • Intervening septum intensity similar to myometrium. Septate uterus • Normal shaped uterus. • Two separate uterine cavity. • Fundal segment of septum with intensity similar to myometrium. • Fibrous segment with low intensity.
- 38. Cont. Arcuate uterus • Normal shaped uterus with single uterine cavity. • Slightly concave or flat external contour. DES related • Small uterus with T-shaped cavity.
- 39. CLASSIFICATION AMERICAN FERTILTY SOCIETY CLASSIFICATION (1988) I. Segmental or complete agenesis or hypoplasia Agenesis and hypoplasia may involve the vagina, cervix, fundus, tubes, or any combination of these structures. Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome is the most common example in this category. II. Unicornuate uterus With rudimentary horn – □ With endometrial cavity- -Communicating -Non communicating □ Without endometrial cavity Without rudimentary horn
- 40. Cont. III. Didelphys uterus • Complete or partial duplication of the vagina, cervix, and uterus characterizes this anomaly. IV. Bicornuate uterus • Complete bicornuate uterus -uterine septum that extends from the fundus to the cervical os. • Partial bicornuate uterus - septum, which is located at the fundus. • In both variants, the vagina and cervix each have a single cavity.
- 41. Cont. V.Septate uterus • A complete or partial midline septum is present within a single uterus. VI. Arcuate uterus • A small septate indentation is present at the fundus. VII. DES-related abnormalities • T-shaped uterine cavity with or without dilated horns is evident. Not associated with renal anomalies.
- 43. Mullerian Agenesis Classified as: Lateral Fusion Defects 1: • most common type of uterine anomalies. • Usually a failure of formation of one Mullerian duct • failure of migration of a duct • failure of fusion of a duct Lateral Fusion Defects 2: Septate Uterus: Contains 2 endometrial cavities but with a normal external surface. Arcuate Uterus:It has a small Septum which can be seen externally as a small indentation at the uterine fundus . Lateral Fusion Defects 3: An asymmetrical lateral fusion defect Unicornate Uterus. The affected mullerian duct does not develop at all or may become a horn of the uterus ( communicating or non-communicating) Can be associated with an an ectopic ovary. This is important with women who are being induced to ovulate.
- 44. Lateral Fusion Defects 4: • Bicornate Uterus :Has two cavities with an indented fundus greater than or equal to 1 cm •. Caused by the partial fusion of the mullerian ducts • Can exist a varying degree of separation Lateral Fusion Defects 5: • Didelphys: Considered a “double uterus” in which 2 mullerian ducts fail to fuse forming 2 uterine cavities. • Limited to the uterus and cervix (no vaginal involvement) •15-20% of patients also have other unilateral anomalies eg; Ipsilateral renal agenesis Vertical Fusion Defects: • defective fusion of the caudal mullerian duct and urogenital sinus • Abnormal vaginal canalization • Symptoms will depend on degree of obstruction of the defect Diethylstilbestrol: It is a synthetic estrogen that was used from 1949-1971 Caused Vaginal adenosis among others… DES induced anomalies of the uterus
- 45. Mullerian Agenesis/Hypoplasia Recently termed- mullerian aplasia. C/by absence or hypoplasia of uterus proximal to vagina & in some cases fallopian tubes. TWO VARIANT □ Partial- rare □ Complete- more common eg: Mayer-Rokitansky-Kuster-Hauser syndrome
- 46. Mayer-Rokitansky-Kuster-Hauser Syndrome Congenital absence of uterus & vagina, small rudimentary uterus may be present. Normal ovarian function including ovulation. Genotype - 46xx. Phenotype – female. Associated with other congenital anomalies- (skeletal, renal).
- 47. Cont. Usually diagnosed at puberty with c/o primary amenorrhea. Age appropriate secondary sexual character. Normal development of breast, body, proportionate hair distribution, external genitalia. Vaginal vault can be either absent completely or short vaginal port can be present. Hormonal profile – Normal.
- 48. Cont. USG • Absence of uterus & fallopian tube with normal ovaries. MRI • Uterus & vagina absent. • Rudimentary uterus can be seen. • Coexisting renal abnormality identified.
- 49. UNICORNUATE UTERUS One mullerian duct develops normally while opposite fails to develop or develop incompletely. With rudimentary horn- □ With endometrial cavity- -communicating -non communicating □ Without endometrial cavity- Without rudimentary horn
- 51. Cont. Associated with urological anomalies-44%. Poorest fetal survival among all mullerian anomalies b/c of – □ Insufficient muscular mass. □ Decreased uterine volume. □ Decreased ability to expand. Non communicating accessory horn having endometrial cavity- most common & most clinically significant. Can cause- hematometra , endometriosis
- 52. Cont. Ectopic pregnancy in horn f/by rupture can happen-should be removed before pregnancy.
- 53. HSG • Useful for diagnosis, • Can not detect non communicating horn. MRI • Reliable. • Only one fallopian tube identified. • Uterine volume reduced • Accessory horn appears solid • Opacified when endometrium is absent.
- 54. USG • Useful for identifying rudimentary horn. • Can identify communication with main uterine cavity.
- 55. Cont Laproscopy Rarely indicated. Additional : IVP, Renal USG Indication of surgery-Presence of accessory horn with endometrium. Laparoscopic hemi hysterectomy of rudimentary horn is treatment of choice.
- 56. UTERINE DIDELPHYS Failure of medial fusion of two mullerian ducts. C/by 2 hemiuterus, 2 endocervical canal, 2 cervix, vagina can be single or double. Each hemiuterus having one fallopian tube. Renal agenesis most commonly associated with uterine didelphys.
- 57. Cont. Simultaneous pregnancy can occur in each uterus –are always dizygotic. Usually asymptomatic (non obstructive) – diagnosed during pelvic examination- two cervix seen. Associated with best possibility of successful pregnancy after arcuate uterus. May have history of recurrent second trimester abortion.
- 58. Unilateral vaginal obstruction can cause hematocolpos, hemetometra, endometriosis- can be overlooked as there is cyclical menstruation from opp. Side.
- 59. Cont. HSG • Two uterine cavity with two cervix with two vagina. • Intercornual distance-> 4 cm. MRI • Two widely separeted uterus. • Two cervix, two vagina. • Associated renal anomaly identified.
- 60. Cont. Indication of vaginal septum resection- Obstructed unilateral hemivagina to preserve fertility. In non obstructive vagina – surgical correction is limited.(severe dyspareunia). Metroplasty – Rarely indicated. Results are disappointing.
- 61. BICORNUATE UTERUS Incomplete fusion at the level of uterine fundus. Lower uterus & cervix are fused completely. Two separate but commmunicating endometrial cavity. Important to differentiate bicornuate uterus from septate uterus –different reproductive outcome & treatment strategies.
- 62. Cont. Subclassification : depending on septum length. COMPLETE : Septum upto cervix. BICORNUATE UNICOLLIS : Septum extends to internal os. BICORNUATE BICOLLIS : Septum extends to external os. PARTIAL : Septum confined to fundal region.
- 63. Complete Partial
- 64. Cont. • Usually don’t have reproductive associated problem. • Depends on length of septum. USG Should be done in luteal phase-endometrial echo complex is better identified. Not useful for distinguising bicornuate uterus form septate uterus.
- 65. Cont. HSG • Not reliable. • Two chambered uterine cavity. • Septal thickness is important. MRI • Two uterine body with single cervix. • Myometrial tissue separating two cavity has intensity identical to that of myometrium.
- 66. Cont. LAPROSCOPY Can distinguish. Surgery seldom required. Preserved for pts. with recurrent spontaneous abortion, preterm birth. Straussmann procedure –treatment of choice.
- 67. SEPTATE UTERUS Failure of resorption of medial septum after complete fusion of mullerian duct. Most common. Subclassification- depending on septal length. COMPLETE : Septum upto os.( double vagina) PARTIAL : Septum does’t extend upto os.
- 68. Fertility is not compromised yet has poorest reproductive outcome. once pregnant, the greater the septum , greater the risk of miscarriage esp. in 2nd trimester. Decreased intrauterine space for fetal growth. Implantation of placenta on poorly vascularized septum. Decision to prefer surgical correction of septum should be based on poor reproductive outcome rather than on presence of septum alone.
- 69. Cont. INDICATION FOR SURGERY • Recurrent spontaneous abortion. • Single 2nd trimester abortion. • Preterm delivery. HSG • Two chambered uterine cavity. • Length & thickness of septa should be assessed.
- 70. Cont. LAPROSCOPY • Best for distinguishing septate from bicornuate uterus. • Normal fundal contour. MRI • Normal fundal contour with outward convexity. • Low signal intensity for septum.
- 71. Cont. Surgical procedure of choice : Hysteroscopy metroplasty with concurrent laparoscopy. (outcomes are excellent) Post t/t miscarriage rates are 10% in contrast to 90% pre t/t rates with complete septum.
- 72. ARCUATE UTERUS Near complete resorption of uterovaginal septum. C/by small intrauterine indentation <1 cm in fundal region. Considered as mild form of bicornuate uterus. Clinically benign.
- 73. HSG • Single uterine cavity with saddle shaped fundal indentation. MRI • Convex or flate contour. • Cavity with broad & smooth indentation similar to myometrium.
- 74. TRANSVERSE VAGINAL SEPTUM Formed when tissue between vaginal plate & caudal aspect of fused mullerian ducts fail to reabsorb. Develop at all levels. a) Superior vagina-46% b) Mid vagina-40% c) Inferior vagina-14%
- 75. Cont. NEONATES & INFANTS Rarely diagnosed in neonates & infants – hydromucocolpos. Unlike imperforate hymen bulging vagina is not seen with valsalva maneuvre. USG is initial study, MRI is more useful as it clearly defines the length of atretic segment between the upper and lower vagina. Management : surgical excision of septum.
- 76. Cont. POST MENARCHAE Symptoms depends on whether septum is complete or incomplete. Presents with primary amenorrhea. Cyclical pelvic pain. O/E Palpable central lower abdominal or pelvic mass secondary to hematometra, hematocolpos, hematosalpinx.
- 77. Cont. Local ex.- no bulging membrane. Incomplete TVS allows menstrual flow to escape periodically but hematometra, hematocolpos can later develop. Temptation to insert a needle for diagnostic purpose must be resisted to avoid the risk of converting a hematocolpos into a pyocolpos Chronic retrograde menstruation frequently result in pelvic endometriosis and adhesions, which can be severe.
- 78. Hematometra
- 80. Imperforate hymen Imperforate hymen is embryologically not of mullerian origin although clinically have a similar presentation Imperforate:[8][9] hymenal opening nonexistent; will require minor surgery if it has not corrected itself by puberty to allow menstrual fluids to escape. Cribriform, or microperforate: sometimes confused for imperforate, the hymenal opening appears to be nonexistent, but has, under close examination, small openings. Septate: the hymenal opening has one or more bands of tissue extending across the opening
- 81. Presenting symptoms Surgical repair after the onset of puberty but before menarche is optimal. The most common scenario is that in which a young woman presents with increasingly severe intermittent abdominal and pelvic pain due to a large hematocolpos and hematometra. This situation is preventable, as routine examinations of the genitalia can detect this obstruction and allow correction before menarche Urinary pressure and even retention, with hydroureter and/or hydronephrosis, may occur due to the mass effect and resultant obstruction. Vaginal and rectal pressure is typically present. Severe constipation and low-back pain are described as presenting symptoms. The laborlike menstrual cramps may be severe and cyclic, although the cyclic nature of the symptoms may not be easily or immediately appreciated by the young woman or her family.
- 82. Cervical Atresia • It is rare • Often presents with normal vagina or absence of lower vagina. • Management of obstruction at the level of cervix is most controversial • conservative approach: uterovaginoplasty • Radical approach: hysterectomy
- 83. a, Isolated congenital cervical atresia with normal vaginal development. b, Congenital cervical atresia with complete vaginal agenesis
- 84. PREGNANCY AND LABOUR IN UTERINE MALFORMATION: •Minor degrees of developmental defects of the uterus do not usually interfere with pregnancy and labour. •In most cases of uterine deformities, the two portions of the uterus and a false decidua may form in the other half. •Abortion does not occur infrequently – in some cases premature labour is the result • In the minor malformations, the pregnancy often goes on to term and ends normally.
- 85. UTERUS BICORNIS BICOLLIS • Pregnancy may occur in either half of the uterus, and when it occurs in one horn of a bicornuate uterus, the other undergoes some degree of hypertrophy and a decidua is formed in its cavity. • Repeated abortions and breech presentations may occur more frequently than in a normal uterus. • Usually, the pregnancy takes a normal course and the delivery is spontaneous •In rare instances, the non pregnancy horn of the uterus may impede the progress of labour by obstructing the passage of the head in the pelvic cavity. • With uterus bicornis unicollis, the difficulty of diagnosis is even greater, and some cases are not diagnosed till after delivery.
- 86. UTERUS DIDELPHYS: • Pregnancy may take a normal course. Occasionally, delivery may be impeded by the septum in the vagina • In the early weeks of pregnancy the presence of the non-gravid uterus may give rise to the mistaken diagnosis of an extrauterine gestation • In some of these cases menstruation may occur throughout the course of pregnancy form the non pregnant uterus. • The pregnancy may be complicated by abortion, preterm delivery, fetal growth restriction and malpresentation.
- 87. UTERUS SEPTUS AND SUBSEPTUS: • In some, pregnancy and labour proceed normally but sometimes repeated abortion may occur • Malpresentations, specially breech, may be more frequent. •In some cases, the placenta may be retained or adherent and it is during the manual removal of the placenta that the condition is generally diagnosed. • In a few cases, the head or part of the fetus may pass through the septum UTERUS UNICOLLIS : • Pregnancy is extremely rare in this type of uterine deformity. Pregnancy in the rudimentary horn is attended with grave risks. • Increased Incidence of abortion, preterm labour, IUGR, breech presentation, uterine dysfunction in labour and caesarean section occur. ARCUATE UTERUS : There is depression at fundus. Fundal notching can be detected at late pregnancy. This results in transverse lie.
- 88. EFFECTS OF ABNORMALITY ON PREGNANCY: •When pregnancy occurs in the woman with an abnormal uterus, the outcome depends on the ability of the uterus to accommodate the growing fetus • If there is insufficient hypertrophy, the possible difficulties are aborton, premature labour and abnormal lie of the fetus.In labour, poor uterine function may be experienced. • Minor defects of structure cause little problem and might pass unnoticed with the woman having a normal outcome to her pregnancy. •Occasionally problems arise when a fetus is accommodated in one horn of a double uterus and the empty horn has filled the pelvic cavity. In this situation the empty horn had grow owing to the hormonal influences of the pregnancy, and its size and position will cause obstruction during labour. Caesarean section would be the method of delivery.
- 89. CLINICAL OUTCOME Gynecological: • Infertility and dyspareunia are often related in association with vaginal septum •Dysmenorrhoea in bicornuate uterus or due to cryptomenorrhoea (pent up menstrual blood in rudimentary horn) • Menorrhagia – due to increased surface area in bicornuate uterus.
- 90. Obstetrical Obstetrical Midtrimester abortion which may be recurrent. Cornual pregnancy – with inevitable rupture around 16 th week – if pregnancy occurs in the rudimentary horn Increased incidence of malpresentation – transverse lie in arcuate or subseptate., breech in biconuate, unicornuate or complete septate uterus Preterm labour Prolonged labour – due to incordinate uterine action Obstructed labour – obstruction by the non-gravid horn of the bicornuate uterus or rudimentary horn Retained placenta and postpartum hemorrhage where the placenta is implanted over the uterine septum.
- 92. VAGINAL AGENESIS Aim:- to create a neovagina. Non surgical Initial therapy. • Frank (1938) described non surgical method to create neovagina using sequential application of wider & longer dilator. • Series of graduated dilator dilate vaginal space. Creates a functional vagina within 3-6 months. • Patient instructed to sit on racing type bicycle seat for at least 2 hrs/day at interval of 15-30 min.(to apply pressure by leaning forward with dilator in place)
- 93. Cont. SURGICAL Non surgical treatment fails-considered. Without use of abdominal contents- Without dissecting cavity- 1. Williams vulvovaginoplasty(1964) 2. Vecchietti procedure(1965) Dissecting cavity & lining with graft- 1. Mc Indoe operation 2. Dermis graft 3. Amnion graft 4. Flaps-Musculocutaneous, fasciocutaneous With use of abdominal contents- • Peritoneum • Intestinal contents.
- 94. Mc Indoe operation- Most common. Most satisfactory results - Procedure of choice. Three important principles- • Dissection of adequate space between bladder & rectum. • Inlay a split thickness skin graft. • Prolonged dilatation during the contractile phase of healing.
- 95. Cont. Technique Skin graft taken. 0.018 inch thick, 8-9 cm wide, 16-20 cm in length. Vaginal form of adequate size is prepared by applying skin graft over it. Neo vaginal space is created. Form placed in neo vagina, edge of graft sutured with skin edge.
- 98. Cont. Post operative management • Bed rest in upright and flat position for one week. • Antibiotics. • Low residue diet. • Replacing with new form-o Removed after 7-10 days. vaginal cavity irrigated with warm saline. o Inspection of cavity to determine the take of graft. o New form applied. o Applied continuously for 6 wks except at the time of urination & defecation. o Next 12 months-new form applied only during night.
- 99. Cont. Complication • Post operative infection. • Intra – post-op hemorrhage. • Post operative fistula formation with solid mould(due to pressure necrosis). rectovaginal-more common • Failure of graft taken up. • Later granulation formation. • Malignant transformation.
- 100. Williams Vulvo vaginoplasty Full thickness skin flap of labia majora to create a vaginal pouch. Advantages- • Technique is simple. • Less local complication. • Early recovery. • Operation of choice for unsatisfactory Mc Indoe operation. • After extensive pelvic surgery or radiation therapy.
- 101. • The Williams vulvovaginoplasty. A horseshoe shaped incision deepened to expose superficial perineal muscle. B:Inner skin margins united progressively with fine sutures. C:vaginal tube completed, admits two fingers and 10-12 cm in length D: The entrance to the pouch should not cover the external urethral meatus.
- 102. VECCHIETTI OPERATION An olive-shaped device placed at vaginal opening and with laparoscopic guidance connected to a traction device on lower abdomen. The traction device is tightened every day, gradually pulling the olive-shaped device inward to create a vagina over about a week. Removal needs further manual dilation.
- 103. UNICORNUATE UTERUS Indication of operation- Presence of endometrium in the accessory horn. Treatment of choice- Laproscopic hemihysterectomy of rudimentary horn. Surgical reconstructive procedures do not improve obstetrical outcome; however cervical cerclage may be beneficial when indicated.
- 104. UTERUS DIDELPHYS Uterus didelphys with obstructed unilateral vagina- Full excision and marsupalization of vaginal septum. Non obstructed- Surgery rarely indicated. Recommended procedure is Strassmann metroplasty in pts with repeated poor obstetrical outcomes
- 105. BICORNUATE UTERUS Seldom requires surgical reconstruction. Treatment of choice – Strassmann procedure. Older procedures – • Jones metroplasty • Thompkins metroplasty
- 106. STRASSMANN METROPLASTY • Incision given in medial side of each hemicorpus, deep enough to enter the endometrial cavity. • The incision extends from the superior aspect of each horn, near the interstitial region of the fallopian tubes, to the inferior aspect of the uterus. • The goal is to achieve a single endocervical canal. If 2 cervices are present, their unification is not recommended.
- 107. Cont. Apposition of the myometrium – After resecting the wedge, the myometrial edges naturally evert. Apposition of the opposing myometrium is achieved using interrupted vertical figure-8 sutures along the posterior and anterior uterine walls. – The final layer is closed using continuous subserosal sutures, without exposing any suture material to the peritoneal cavity. – Transvaginal dilatation of the cervix is performed, assuring proper endometrial cavity drainage.
- 108. The Strassmann metroplasty with modification. A: If a rectovesical ligament is found, it should be removed. B: An incision is made on the medial side of each hemicorpus and carried deep enough to enter the uterine cavity. The edges of the myometrium will evert to face the opposite side. C and D: The myometrium is approximated by use of interrupted vertical figure-of-eight 3—0 polyglycolic acid sutures. One should avoid placing sutures too lose to the interstitial portion of the fallopian tubes. E: A continuous 3—0 polyglycolic acid subserosal suture is used as a final layer. Tourniquets are removed, and defects in the broad ligament are closed.
- 109. Jones Metroplasty • Abdominal approach. • Wedge shaped incision given at the top of fundus within 1 cm of insertion of tubes. • Uterine septum excised as wedge. • Unification of two halves of uterus is done in three layers with interrupted stitches.
- 110. THOMPKINS METROPLASTY • Abdominal approach. • Single median incision given- divides uterine corpus in half. • Each lateral half incised to within 1 cm of tubes. • Myometrium is reapproximated. • Leaves the uterotubal junction in a more normal and lateral position. • Less traumatic and cause less bleeding
- 111. SEPTATE UTERUS Indication of surgery- • Recurrent spontaneous abortion • History of preterm labour. Procedure of choice- Transcervical hysteroscopic lysis of uterine septum with concurrent laproscopy. Preoperatively GnRH analogues for 2 months are given to induce endometrial atrophy.
- 112. Cont. • The laparoscope is placed. • Hysteroscopy commences,and the hysteroscope is inserted to the level of the external os. • Using an Operating continous flow hysteroscope, the septum may be divided with diathermy scissors, a rectoscope wire or knife electrode or the Nd YAG laser. Dissection of the septum is complete when the hysteroscope can be moved freely from 1 tubal ostium to the other . – the tubal ostia are visualized simultaneously, – and bleeding occurs from small vessels at the fundal myometrium.(septum is relatively avascular)
- 113. Cont. Main complication is Uterine perforation Fluid overload Post op management- • Placement of intrauterine device for a month - controversial. • Conjugated estrogen and progesteron added to facilitate epithilelization. • After one month follow with HSG & Hysteroscopy.
- 114. TRANSVERSE VAGINAL SEPTUM Cont. Excision Of septum followed by vaginoplasty. Depends on location & thickness of septum. High TVS Surgical correction is more difficult. Transverse incision made in vaginal vault. Dissection done between bladder & rectum upto cervix. Lateral margin of septum excised. Hematocolpos drained. And form channel for drainage, placed in vagina- allows epithelialization & maintains patency.
- 116. Cont. LOW, MID, THIN TVS Excised with multiple radial incision. Upper & lower segments joined with multiple delayed absorbable sutures. Because septa that appears relatively thin may be significantly larger after decompression of the proximal haematcolpus, consider the possibility that a graft may be required.
- 117. • Surgical correction of transverse vaginal septum. A: The upper end of a short vagina. The small sinus tract opening, through which the patient menstruated, is shown. The line of incision is drawn through the mucous membrane between the vaginal dimple and the sinus. B: Areolar tissue is dissected through to the pocket of mucosa that covered the cervix. The mucosa is incised. C: An anastomosis is made between the lower vagina and the upper vagina. 0: Completed vagina. It is slightly shorter than normal but of normal caliber.
- 118. Vaginal atresia
- 119. Hymenotomy The objective of a hymenotomy procedure is to open the hymenal membrane in such a way as to leave a normally patent vaginal orifice that does not scar The hymenal orifice is enlarged using a circular incision following the lines of the normal annular hymenal configuration. Alternatively, a cruciate incision along the diagonal diameters of the hymen, rather than anterior to posterior, avoids injury to the urethra and can be enlarged by removal of excess hymenal tissue. In either approach, hemostasis is required using interrupted stitches with fine absorbable suture (eg, 4-0 polyglycolic acid suture). The surgical procedure of hymenotomy and evacuation of hematocolpos is performed in an outpatient setting. The patient and family should be instructed to expect continued drainage of dark, thick, old blood for several days to a week after the procedure. Mild cramping may occur as the hematometra resolves and evacuates.
- 121. COMPLICATIONS of MULLERIAN ANOMALIES Abortion Weak uterine action Post partum hemorrhage Adhesion of the placenta Malpresentations Prolonged or obstructed labour Uterine rupture due to its poor development. The placenta, if it is formed on the septum, may be adherent and may cause post partum hemorrhage.
- 122. CONCLUSION Müllerian anomalies are a morphologically diverse group of developmental disorders that involves the internal female reproductive tract. Establishing an accurate diagnosis is essential for planning treatment and management strategies. The surgical approach for correction of müllerian duct anomalies is specific to the type of malformation and may vary in a specific group. For most surgical procedures, the critical test of the procedure's value is the patient's postoperative ability to have healthy sexual relations and achieve successful reproductive outcomes.
- 123. oUterine malformations like absence, rudimentary or infantile are not amenable to treatment. o Hypoplastic uterus in young girls may gradually develop with advance of age. o Oestrogen therapy may be temporarily given for amenorrhea, oligomenorrhoea o dilation and curettage may be helpful in some cases with dysmenorrhoea. oChance pregnancy may develops in the hypoplastic uterus oCervical cerclage is indicated in women with uterine didelphys, unicornuate or bicornuate uterus and poor reproductive performance.
- 124. Thank you