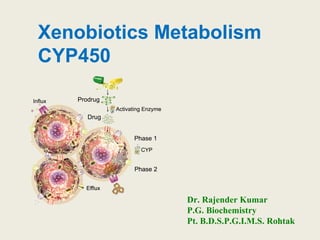
CYP450 Xenobiotics Metabolism
- 1. Xenobiotics Metabolism CYP450 Dr. Rajender Kumar P.G. Biochemistry Pt. B.D.S.P.G.I.M.S. Rohtak
- 2. Introduction A xenobiotic is a foreign chemical substance found within an organism that is not normally, naturally produced by or expected to be present within that organism. It can also cover substances which are present in much higher concentrations than are usual Examples- Drugs, food additives, pollutants, insecticides, chemical carcinogens etc They enter body mainly with food or as medications Three principal entries: intestine, lungs, skin
- 3. Entry of xenobiotic into cells • Simple diffusion – lipophilic substances, depends on concetration gradient (liver – freely permeable, big pores in cell membrane, most affected in poisoning) • Facilitated diffusion – transporters • Active transport – primary, secondary • Endocytosis • xenobiotics structurally similar with physiological substrates can utilize all available transport systems
- 4. Excretion of xenobiotics from cell • primary active transport – needs energy: ATP hydrolysis • special ATP-ases called ABC (ATP binding cassettes) localized in cell membranes, export xenobiotics from cells into ECF • MRP (multidrug resistance proteins) – in increased expresion, they cause the resistance towards medicines
- 5. Excretion of xenobiotics from body • chemically modified (more polar) xenobiotics are excreted by urine, bile, stool, or sweat • volatile substance by lungs • excretion into human milk • intestinal deconjugation and reabsorption sometimes occur - enterohepatic circulation
- 6. Biotransformation and detoxification Biotransformation is Conversion of lipophilic to water- soluble chemicals catalyzed by enzymes in the liver and other tissues In most cases, biotransformation lessens the toxicity of xenobiotics The term “detoxification” is sometimes used for many of the reactions involved in the metabolism of xenobiotics
- 7. Increasingly humans are subjected to exposure to various foreign chemicals xenobiotics. Knowledge of the metabolism of xenobiotics is basic to a rational understanding of pharmacology and therapeutics pharmacy toxicology management of cancer, and drug addiction All these areas involve administration of, or exposure to, xenobiotics Biomedical importance
- 8. 1. facilitates excretion: Converts lipophilic to hydrophilic compounds 2. Detoxification/inactivation: converts chemicals to less toxic forms 3. Metabolic activation: converts chemicals to more toxic active forms or converts inactive drug to its active form Purpose of Biotransformation
- 9. Sites of biotransformation • Liver – Primary site! Rich in enzymes – Acts on endogenous and exogenous compounds • Extrahepatic metabolism sites – Intestinal wall • Sulfate conjugation • Esterase and lipases - important in prodrug metabolism – Lungs, kidney, placenta, brain, skin, adrenal glands
- 10. Metabolism of Xenobiotics phase 1 1. Hydroxylation Monooxygenases or cytochrome P450s Hydroxylation may terminate the action of a drug 2. deamination, dehalogenation, desulfuration, epoxidation, peroxygenation, and reduction, hydrolysis • Purpose – Introduction of polar functional groups in a molecules ♣ Increase a molecule’s polarity ♣ Does provide a site for phase II metabolism
- 11. Metabolism of Xenobiotics Phase 2 conjugation with glucuronic acid, sulfate, acetate, glutathione, methyl or certain amino acids, The overall purpose of phases II of metabolism of xenobiotics is to increase their water solubility (polarity) and thus excretion from the body
- 12. Xenobiotic-Metabolizing Enzymes (XME) Phase 1 • Cytochromes P450 • Flavin Containing Monooxygenase • Epoxide Hydrolase • Alcohol /Aldehyde Dehydrogenases • Monoamine Oxidases • Xanthine oxidase Phase 2 “Transferases” Sulfotransferases (ST) UDP-glucuronosyltransferases (UGT) Glutathione S-transferases (GST)
- 13. Cytochrome P450 • superfamily of heme enzymes (many isoforms) can catalyze different reaction types, mainly hydroxylation • Human:18 families, 43 subfamilies, 57 sequenced genes • can be induced and inhibited • occur in most tissues (except of muscles and erythrocytes) • the highest amount in the liver (ER) • exhibit genetic polymorphism (atypical biotransformations) • Nomencleature: CYP1A2 family subfamily individual member of that subfamily
- 14. Location of Cytochrome P450
- 17. • They are present in highest amount in liver and small intestine but are probably present in all tissues • In liver and most other tissues, they are present mainly in the membranes of the smooth endoplasmic reticulum • In the adrenal, they are found in mitochondria as well as in the endoplasmic reticulum • The various hydroxylases present in that organ play an important role in cholesterol and steroid biosynthesis Cytochrome P450
- 18. • At least six isoforms of cytochrome P450 are present in the endoplasmic reticulum of human liver, • acting on both xenobiotics and endogenous compounds • P450 metabolizes certain widely used solvents and also components found in tobacco smoke, many of which are established carcinogens • Most isoforms of cytochrome P450 are inducible • Induction of cytochrome P450 has important clinical implications, since it is a biochemical mechanism of drug interaction Cytochrome P450
- 19. Certain isoforms of cytochrome P450 (eg, CYP1A1) are particularly involved in the metabolism of polycyclic aromatic hydrocarbons (PAHs) and related molecules for this reason they were formerly called aromatic hydrocarbon hydroxylases (AHHs) This enzyme is important in the metabolism of PAHs and in carcinogenesis produced by these agents Cytochrome P450
- 21. Certain cytochrome P450s exist in polymorphic forms (genetic isoforms), some of which exhibit low catalytic activity CYP2A6 involved in the metabolism of nicotine to conitine, three alleles have been identified, a wild type and two null or inactive alleles Individuals with the null alleles, who have impaired metabolism of nicotine, are apparently protected against becoming tobacco- dependent smokers because their blood and brain concentrations of nicotine remain elevated longer It has been speculated that inhibiting CYP2A6 may be a novel way to help prevent and to treat smoking Cytochrome P450
- 22. • some xenobiotics induce the synthesis of CYP – the metabolic capacity of CYP is enhanced • if administered inducer + drug, both metabolized by the same CYP isoform and drug is metabolized faster, drug is less effective • some xenobiotics inhibit CYP • the most common isoform CYP3A4 metabolizes more than 120 different pharmaceutical drugs • inhibitors of CYP3A4 are e.g. macrolide antibiotics, grapefruit (furanocoumarins), ketoconazole • if administered inhibitor + drug, increased drug level, overdosing , side effects Inducers and inhibitors of CYP450
- 23. cytochrome P450 contains three cofactors and two enzymes: • NADPH+H+, FAD, heme • NADPH:CYP reductase (separates 2 H 2 e- + 2H+) and cytochrome P-450 hydroxylase Lipids are also components of the cytochrome P450 system The preferred lipid is phosphatidylcholine, which is the major lipid found in membranes of the endoplasmic reticulum Components of cytochrome P450
- 24. Mechanism of CYP hydroxylation The formation of hydroxyl group monooxygenase: one O atom from O2 molecule is incorporated into substrate between C and H (R-H → R-OH ) The second O atom + 2H from NADPH+H+ give water R-H + O2 + NADPH + H+ → R-OH + H2O + NADP+ 2 e- + 2 H+
- 25. Mechanism of CYP hydroxylation
- 27. • Hydroxylation is the chief reaction involved • The responsible enzymes are called monooxygenases and cytochrome P450s • Hydroxylation by CYP450 occurs in endogenous and exogenous substrates • Endoplasmic reticulum: squalene, cholesterol, bile acids, FA desaturation, prostaglandins, xenobiotics • Mitochondria: steroidal hormones hydroxylation
- 30. Flavin-containing Monooxygenase •FAD-containing monooxygenases (FMO) oxidize nucleophilic nitrogen, sulfur and phosphorus heteroatoms of a variety of xenobiotics • FMO’s are not inducible and are constitutively expressed •Can be inhibited by other substrates • Located in microsomal fraction of liver, kidney, and lung FMO FAD FMO FADH2 NADP + FMO FADHOOH NADP+ FMO FADHOH NADP+ NADPH + H+ O2 X XO NADP+ H2O FADHOOH is 4a-hydroperoxyflavin FADHOH is 4a-hydroxyflavin FMO FAD
- 31. FMO Example Reactions N N CH3 N N CH3 excretion nicotine O N O CH3 H N O CH3 OH nicotine-1'-N-oxide 2-acetylaminofluorene (2-AAF) caricnogen N-hydroxy-2-AAF FMO FMO
- 32. Epoxides are highly reactive and mutagenic or carcinogenic can form during Phase I (CYP/COX) Epoxide hydrolase converting them into much less reactive dihydrodiols There are 5 distinct forms of EH in mammals: 1. Microsomal epoxide hydrolase (mEH) 2. Soluble epoxide hydrolase (sEH) 3. Cholesterol epoxide hydrolase 4. LTA4 hydrolase 5. Hepoxilin hydrolase mEH and sEH hydrolyze xenobiotic epoxides while the latter 3 hydrolases act on endogenous substrates Epoxides
- 33. Hydrolysis in plasma by esterases (suxamethonium by cholinesterase) Alcohol and aldehyde dehydrogenase in liver cytosolic (ethanol) Monoamine oxidase in mitochondria (tyramine, noradrenaline, dopamine, amines) Xanthine oxidase (6-mercaptopurine, uric acid production) Enzymes for particular substrates (tyrosine hydroxylase, dopa-decarboxylase etc.) Other (non-microsomal) Phase I reactions
- 34. RCH2NH2+O2+H2O2 RCHO+NH3+H2O •MAO catalyze the oxidative deamination of monoamines •Oxygen is used to remove an amine group from a molecule, resulting in the corresponding aldehyde and ammonia • MAO are found bound to the outer membrane of mitochondria in most cell types in the body •They belong to protein family of flavin containing amine oxidoreductases Non-Microsomal Oxidation Reactions
- 35. Hydrolytic Reactions R1 R2 Name Susceptibility to Hydrolysis C O Ester Highest C S Thioester O O Carbonate C N Amide O N Carbamate N N Ureide Lowest Naming carbonyl - heteroatom groups Hydrolyzes (adds water to) esters and amides and their isosteres Enzymes: Non-microsomal hydrolases however amide hydrolysis appears to be mediated by liver microsomal amidases, esterases, deacylases R1 C R2 O δ− δ+ O CH3 CO2H O OH CO2 H CH3 O OH ASA Acetylsalicylic Acid esterase
- 38. Glucuronidation • most frequent conjugation reaction. • UDP-glucuronic acid (UDPGA) is the glucuronyl donor • UDP-glucuronyl transferases (UGT), present in both the endoplasmic reticulum(ER) and cytosol, are the catalysts • Molecules such as 2-acetylaminofluorene (a carcinogen), aniline, benzoic acid, meprobamate (a tranquilizer), phenol, and many steroids are excreted as glucuronides • The glucuronide may be attached to oxygen, nitrogen, or sulfur groups of the substrates
- 39. Glucuronidation
- 41. Some alcohols, arylamines, and phenols are sulfated other biologic sulfation reactions are sulfation of steroids, glycosaminoglycans, glycolipids, and glycoproteins The sulfate donor is adenosine 3-phosphate-5- phosphosulfate (PAPS) Leads to inactive water-soluble metabolites Sulfation
- 42. Glutathione (γ-glutamyl-cysteinylglycine) is a tripeptide consisting of glutamic acid, cysteine, and glycine It detoxify electrophilic chemicals Conjugation with Glutathione
- 43. The glutamyl and glycinyl groups belonging to glutathione are removed by specific Enzymes acetyl group (donated by acetyl- CoA) is added to the amino group of the remaining cysteinyl moiety The resulting compound is a mercapturic acid, a conjugate of L acetylcysteine, which is then excreted in the urine Mechanism Conjugation with Glutathione
- 44. Reaction catalyzed by acetyltransferases present in the cytosol of various tissues, particularly liver Important for drugs with primary amino groups The drug isoniazid, used in the treatment of tuberculosis, is subject to acetylation Acetylation does NOT increase water solubility Causes Detoxification or termination of drug activity Acetylation isoniazid
- 45. A few xenobiotics are subject to methylation by methyltransferases S-adenosylmethionine is methyl donor Key for biosynthesis of many compounds Important in the inactivation of physiologically active biogenic amines neurotransmitters norepinephrine, dopamine, serotonin, histamine Minor pathway in the metabolism of drugs Methylation does NOT increase water solubility Most methylated products are inactive Methylation
- 47. • with glycine, taurine • xenobiotics with -COOH groups are the substrates • endogenous example: conjugated bile acids Approximately 76% of aspirin is metabolized through amino acid conjugation Salicyluric acid, the glycine conjugate of salicyclic acid, is the main metabolite of aspirin Conjugation with amino acids
- 48. Peroxidases RH + O2 PHS R-OOH + X or XH PHS MOx LOx ROH + XO or X R-OOH + carcinogen PHS MOx LOx active carcinogen (ie. aflatoxin) 1. Prostaglandin H synthase (PHS, COX1,2) (brain, lung, kidney, GI tract, urinary bladder) 2. Myeloperoxidase (MOx) (leukocytes) 3. Lactoperoxidase (LOx) (mammary gland) Most oxidative biotransformations require reduced cofactors NADPH and NADH, except for peroxidases that couple the reduction of hydrogen peroxide and lipid hydroperoxides to the oxidation of other substrates called cooxidation
- 49. Prostaglandin H synthase COOH arachidonic acid O2 + O2 O O COOH OOH PGG2 cyclooxygenase peroxidase X or 2XH XO or 2X + H2O O O COOH OH PGH2 prostacyclinthromboxane A2prostaglandins (PGD2, PGE2) PHS (COX) has two catalytic activities: 1. a cyclooxygenase (COX) that converts arachidonic acid to the cyclic endoperoxide- hydroperoxide PGG2) 2. a peroxidase (that converts the hydroperoxide to the corresponding alcohol PGH2) which can result in the oxidation of xenobiotics 3. COX-2 inhibitors include aspirin and ibuprofin PHS can bioactivate carcinogens such as β- napthylamine, a bladder carcinogen NH2 PHS NH DNA damage
- 55. CARCINOGENS
- 56. PAHs formed by: - incomplete combustion of organic matter such as coal, wood, oil, petrol and diesel - coke production, vehicle and aircraft exhaust - smoking cigarettes - charbroiled meats PAHs are also found in natural fuel deposits A few PAHs are used to produce medicine, dyes, plastics, & pesticides Natural sources of PAHs include volcanoes and natural fires Examples include Benzo(a)pyrene and Benzo(b)fluoranthene PAH in environment
- 57. - radicals formed by pyrolysis of hydrocarbons between 500 and 800ºC in zone of flame with insufficient O2 - C1 and C2 fragments combine in reducing atmosphere to form condensed aromatics - on cooling, PAHs condense onto existing particles – their distribution reflects their differing thermodynamic stability in O2 deficient flame Mechanism of formation during combustion Source % Heating, power production 51 Industrial producers 20 Incineration & open burning 28 Vehicles 1 B(a)P in foodstuffs μg/kg Charcoal broiled steak 8 Margarine 1-36 Sausages 4-50 Roasted coffee 1-13 Toast 0.5
- 58. PAHs effects •Some PAHs have been shown to be cancer causing •Chronic Bronchitis •Skin Problems •Allergies Fetus is at greater risk and susceptibility : •Growth retardation •Low birth weight •Small head circumference •Low IQ •Damage DNA •Disrupt endocrine systems, such as estrogen, thyroid, and steroids
- 59. CYP/PHS O EH HO OH CYP/PHS HO OH O benzo[a]pyrene (+) benzo[a]pyrene 7,8-oxide (-) benzo[a]pyrene 7,8-dihydrodiol (+) benzo[a]pyrene 7,8-dihydrodiol-9,10-epoxide ULTIMATE CARCINOGEN HN N N NO HN DNA HO OH HO BaP-N2 -dG DNA adduct DNA GST/GSH OH GS inactive (excreted) O CYP/PHS OH OH inactive Phase II Phase II and excretion PAHs metabolites
- 60. • The first reaction is an epoxidation. With benzo(a)pyrene, the product is the corresponding 7,8-epoxide that, in turn, is subject of epoxide hydrolases to form stereoisomeric dihydrodiols • These are converted further to the 7,8-dihydrodiol-9,10- epoxide. The terminal oxidase is cytochrome P-450 (CYP1A1). The diol epoxide can exist in 4 stereoisomeric forms of which the key carcinogenic product is benzo(a)pyrene-r-7,t-8-diol-t-9,10-epoxide • PAH epoxides can then be conjugated with GSH. This conjugation is regarded as a true detoxification reaction and is mediated by glutathione transferase (GSTM1) PAHs metabolites
- 61. • The epoxides that are not conjugated with GSH are converted into phenols and diols. These PAH metabolites, however, are sometimes not sufficiently polar to be excreted and are therefore conjugated with glucuronic or sulfuric acids to enable excretion to occur • In addition to conjugation, the hydroxylated derivatives of PAHs may undergo a number of oxidation and hydroxylation reactions. These include the conversion of phenols to phenol-epoxides and subsequently to diphenols and triols, diols to tetrols and diol-epoxides, and triols to triolepoxides and pentols PAHs metabolites
- 62. Aflatoxin Aflatoxins are naturally occurring mycotoxins that are produced by many species of Aspergillus, a fungus. They can be found on moldy peanuts, rice, corn and other crops. Aflatoxin B1 is the most potent liver carcinogen. Aspergillus fungus that procues aflatoxin Aspergillus fungus on corn
- 63. O O O OO OCH3 * * isolated e- -rich double bond aflatoxin O O O OO OCH3 * * O ULTIMATE CARCINOGEN CYP/PHS DNA NHN N N O NH2 DNA O O O OO OCH3 HO GST/GSH O O O OO OCH3 * *GS OH EH inactive (excreted) O O O OO OCH3 * *HO OH * * AFB1 N7-DNA adduct * electrophilic some DNA activity Epoxide hydrolase can detoxify aflatoxin-epoxide from binding to DNA, but still has some mutagenic activity Aflatoxin metabolism
- 64. N-Hydroxylation of AAF N-Hydroxylation of AAF is the first metabolic step towards the development of a carcinogenic agent
- 65. Further Metabolism of N-HydroxyAAF Produces Cancer N-HydroxyAAF undergoes phase II metabolism to the ultimate carcingogen. The glucuronide pathway is also involved in carcinogenesis
- 66. Tobacco
- 67. • during cigarette burning? • temperature about 900 o C • dried tobacco undergoes incomplete combustion • nicotine partly passes to smoke, partly decomposes • Nicotine: 0.9 mg/cig. • Tar: 11 mg/cig. Tobacco
- 68. Cigarette smoke contains • free base of nicotine – binds to receptors in the brain • CO – binds to hemoglobin to give carbonylhemoglobin (tissue ischemia) • nitrogen oxides – may generate reactive radical species • polycyclic aromatic hydrocarbons (PAH)(pyrene, chrysene, benzo[a]pyrene …), main components of tar • they can attack and damage DNA, carcinogens • other substances (N2, CO2, HCN, CH4, esters …) Tobacco
- 70. Toxic effects of xenobiotics 1. cell injury (cytotoxicity) 2. the reactive species of a xenobiotic may bind to a protein, altering its antigenicity. The xenobiotic is said to act as a hapten 3. reactions of activated species of chemical carcinogens with DNA are thought to be of great importance in chemical carcinogenesis
- 71. Factors that influence metabolism of xenobiotics • Age – older people less efficient at metabolism • Sex – Linked to hormonal differences • Heredity – Genetic differences can influence amounts and efficiency of metabolic enzymes • Disease states – Liver, cardiac, kidney disease
- 72. THANKS
Editor's Notes
- Primary active transporters most commonly use adenosine triphosphate (ATP) as an energy source for substrate transport. Secondary active transporters use the concentration gradient of another substance, such as protons or sodium ions, but also other ionic endogenous substances as energy sources to drive transport.
- Types of ATPases P-type (Ca and Na/K pumps) Asp phosphorylation 10 transmembrane domains F-type (Proton pumps) Multisubunit complexes Reversible ABC (ATP binding cassettes) Mechanism unknown
- Subcellular Locations of Metabolizing Enzymes ENDOPLASMIC RETICULUM (microsomes): the primary location (a) Phase I: cytochrome P450, flavin-containing monooxygenase, aldehydeoxidase, carboxylesterase, epoxide hydrolase, prostaglandin synthase, esterase. (b) Phase II uridine diphosphate-glucuronosyltransferase, glutathione S-transferase, amino acid conjugating enzymes. CYTOSOL : many water-soluble enzymes. (a) Phase I: alcohol dehydrogenase, aldehyde reductase, aldehyde dehydrogenase, epoxide hydrolase, esterase (b) Phase II: sulfotransferase, glutathione S-transferase, N-acetyl transferase, catechol 0-methyl transferase, amino acid conjugating enzymes MITOCHONDRIA (a) Phase I: monoamine oxidase, aldehyde dehydrogenase, cytochrome P450 (b) Phase II: N-acetyl transferase, amino acid conjugating enzymes LYSOSOMES :Phase I: peptidase. NUCLEUS: Phase II: uridine diphosphate-glucuronosyltransferase (nuclear membrane of enterocytes)
- An epoxide is a cyclic ether with three ring atoms. These rings approximately define an equilateral triangle, which makes it highly strained. The strained ring makes epoxides more reactive than other ethers. EH is inducible by 2-3 fold by: CYP inducers (PAH, TCCD) EH is inducible by 10-fold by antioxidants BHA, BHT
- Two MAOs have been identified: MAO–A and MAO–B. Equal amounts are found in the liver, but the brain contains primarily MAO–B MAO–A is found in the adrenergic nerve endings MAO–A shows preference for serotonin, catecholamines, and other monoamines with phenolic aromatic rings MAO–B prefers non–phenolic amines b–Phenylisopropylamines such as amphetamine and ephedrine are not metabolized by MAOs but are potent inhibitors of MAOs
- Glutathione – three functions • Reduction- antioxidant (glutathione peroxidase) • Conjugation -(glutathione transferase) • AA Transport into cells -(glutamyltransferase, GMT) A number of potentially toxic electrophilic xenobiotics (such as certain carcinogens) are conjugated to the nucleophilic GSH The enzymes catalyzing these reactions are called glutathione S transferases and are present in high amounts in liver cytosol and in lower amounts in other tissues
- Other metabolites of aspirin the acyl glucuronide conjugate of salicylic acid (salicylic acid glucuronide) the phenol glucuronide conjugate of salicylic acid (salicyl phenol glucuronide) the ring hydroxylated product of salicylic acid (gentisic acid) the ring hydroxylated product of the glycine conjugate (gentisuric acid
- Cancers associated with exposure to PAHs-containing mixtures are predominantly lung and skin cancers,following inhalation and dermal exposure, respectively. Bladder cancer has also been associated with exposure to PAHs in aluminium plants or when handling asphalt
