Cutaneous malignancies
- 1. Cutaneous Malignancies -Dr. Harish Kumar Kabilan
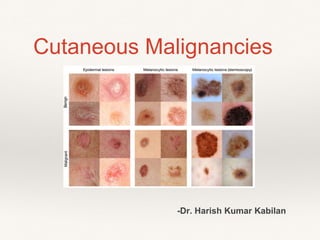
- 4. ❖ Benign Classification of skin tumours ❖ o Squamous cell carcinoma. o Basal cell carcinoma. o Melanoma. o Malignant skin adnexal tumour. o Secondaries in the skin.. ❖Malignant o Seborrhoeic keratosis. o Trichilemmal tumour. o Sebaceous adenoma. o Sebaceous epithelioma. o Hydrocystoma, syringoma, spiradenoma. •Melanoma •Non melanoma cutaneous malignancies
- 5. PATHOPHYSIOLOGY OF THE SKIN AND SUBCUTANEOUS TISSUES RADIATION DAMAGE: Ultraviolet radiation (UVR) and ionising radiation (IR) damage cellular DNA via the tumour suppressor gene p53. UV RADIATION: UVR is divisible into A, B and C according to wavelength. UVR is the principal cause of skin cancer in all skin types IONISING RADIATION: it is dose and time dependent.
- 6. Ultraviolet light UV A – 320nm-400nm B – 290nm-320nm C – 100nm-280 nm
- 7. .UVA contributes to skin cancer via indirect DNA damage (free radicals such as reactive oxygen species). UVB photons can cause direct DNA damage. As a defense against UV radiation, the amount of melanin in the skin increases when exposed to moderate levels of radiation.
- 9. Benign lesions 1.Basal cell papilloma (seborrhoeic keratosis, senile keratosis, verruca Senilis) 2.Papillary wart (verruca vulgaris) SKIN LESIONS 3.Freckle (ephilis)
- 11. 7.Spitz naevus 8.Spindle cell naevus 9.Halo naevus 10.Café-au-lait spots
- 12. 11.Mongolian spot 12.Blue naevus 13.Naevi of Ota and Ito
- 13. Premalignant lesions 1.Actinic/solar keratosis 3.Keratoacanthoma 4.Bowen’s disease . 2.Cutaneous horn
- 14. 5.Extramammary Paget’s disease 6.Giant congenital pigmented naevus or giant hairy naevus 7.Dysplastic (atypical) naevus
- 15. CHARACTERISTICS OF A DYSPLASTIC NAEVUS ❖ Asymmetry ❖ Border- Irregular/ poorly defined ❖ Colour - Variable. Tan brown/black. Red ❖ Blue, white ❖ Diameter - >6mm ❖ Evolving in color/size/ shape
- 16. CONGENITAL/ GENETIC SYNDROMES Naevoid basal cell carcinoma (Gorlin’s) syndrome Xeroderma pigmentosum .
- 17. Gardner’s syndrome Ferguson-Smith syndrome
- 18. ❖ Malignant melanoma (MM) accounts for 3 per cent of all malignancy worldwide. It is the most common cancer in young adults (20–39 years) and the most likely cause of cancer-related death. MALIGNANT LESIONS CUTANEOUS MELANOMA
- 19. Pathophysiology Clark’s concept—Two phases of growth: Initial radial growth phase occurs horizontally, later vertical growth phase occurs with invasion. UV exposure is the major causal factor for developing MM.
- 20. Risk Factors o Exposure to sunlight (exposure to UV light; more common in white-skinned—20 times). o Ethnic factors,socioeconomic status(highsociety),lifestyle, climate. o Albinism. o Xeroderma pigmentosa o Junctional naevus. o Familial dysplastic naevus syndrome. o Sporadic dysplastic naevi. 10% risk. o Large congenital naevi (larger than 20 cm). o Family history of melanoma o History of earlier skin cancers other than melanoma. o Patients who are on immunosuppressive drugs or after renal transplantation or NHL
- 21. Examination• History • high-risk skin type a history of severe blistering sunburns, • intense intermittent sun exposure, • upper socioeconomic status, • family history of melanoma, • large number of nevi, • giant congenital nevi, • presence of dysplastic nevi, • immunosuppression, • history of prior melanoma or other skin cancers • xeroderma pigmentosum.
- 22. • Non painful, itchy lesion, in sun exposed sites, with a recent change in colour/ size, sometimes with ulcer formation often covered with a crust. • Bleeding and sub acute infection is common. • Firm in consistency. The ulcer may need easily on touch • The regional lymph nodes are involved quite early and these are almost always enlarged when the patient presents to the surgeon. Nodes are also hard to firm in consistency • Satellite nodules may be seen in the skin and subcutaneous tissue between the primary tumour and the nearest regional lymph nodes. Typical Presentation
- 23. Physical examination Asymmetry Border- Irregular/ poorly defined Colour - Variable. Tan brown/black. Red Blue, white Diameter - >6mm Evolving in color/size/ shape
- 24. Glasgow criteria:Major signs: Change in size (diameter more than 6 mm), shape and colour • Other changes: Inflammation, crusting, bleeding, itching Nodularity, ulceration, halo around a mole Satellite lesions Doppler positive pigmented lesions using hand held Doppler ( > 1 mm thick lesion)
- 25. 3. Lentigo maligna melanoma: TYPES 2. Nodular melanoma: 12-25%. 4. Acral lentiginous melanoma: 6. Desmoplastic melanoma5. Amelanotic melanoma:
- 26. Familial Melanoma There may also be a family history of other malignancies, especially pancreatic cancer. They require detailed dermatologic evaluation several times annually, with periodic biopsies of the most suspicious lesions. Mutations in the gene CDKN2A in the 9p21 region CDK4
- 27. o No incision biopsy. It can cause early blood spread. o Excision biopsy of primary. It is done with 2 mm margin with deeper fatty tissue. o FNAC of lymph node. o U/S abdomen to look for liver secondaries (usually huge hepatomegaly occurs). o Chest X-ray to look for secondaries in lung (“cannon ball” appearance). HRCT of chest is ideal. o Relevant other methods depending on site and spread, e.g. CT scan of head, chest, abdomen, pelvis. o Urine for melanuria signifies advanced disease. o Sentinel lymph node biopsy (SLNB). Investigations
- 30. Classifications Clark’s levels Level 1: Only in epidermis Level 2: Extension into papillary dermis Level 3: Filling of papillary dermis completely Level 4: Extension into reticular dermis Level 5: Extension into subcutaneous tissue Relation of Tumour Thickness to Nodal Spread— Based on AJCC Classification
- 31. Breslow’s classification (1970): Based on thickness of invasion measured by optical micrometer—most important prognostic indicator until nodal spread I: Less than 0.75 mm II: Between0.76to1.5mm III: 1.51 mm to 4 mm IV: more than 4 mm
- 32. Treatment For Primary: a. Handley’s wide local excision (WLE) is wide excision with clearance of margin as well as depth. b. Primary closure or SSG or local flaps are used to cover the defect. b. In fingers and toes, disarticulation is required. 1 joint above. c. Melanoma in anal canal may require abdominoperineal resection. d. Enucleation in case of melanoma in eye.
- 35. For lymph node secondaries: 1.In a clinically palpable lymph node, FNAC of lymph node is done. 2.In a fixed lymph node, only chemotherapy is the treatment because it is inoperable. 3.Lymphatic mapping and sentinel node biopsy SLNB is useful for melanoma with thickness more than 1 mm depth. 4.Prophylactic regional block dissection - not done anymore. 5. Management in unknown primary (2%) presenting as nodal secondaries is by nodal radical dissection at the region with adjuvant chemotherapy. T
- 36. A vital blue dye (e.g., isosulfan blue) is injected into the dermis around the melanoma site. It is combined lymphatic mapping technique allows for the identification of the sentinel nodes in 99% of patients It is injected just before the operation. it is best to inject it within the margins of the planned WLE. A hand-held gamma probe is used to identify the location of the sentinel node(s), and dissection is performed to identify blue lymphatic channels entering into a blue, radioactive lymph node, which is removed SLN biopsy
- 37. The only adjuvant therapy approved by the U.S. Food and Drug Administration (FDA) is high-dose inte Interferon alfa-2b is administered at a dose near the maximally tolerated dose, with 1 month of IV thera Adjuvant Therapy Systemic therapy
- 39. Stage 0, I, and IIA - followed by history and physical examination at least every 6 months for the first 3 For stage IIB, IIC, and III melanoma patients, history and physical examination every 3 or 4 months fo For patients with stage IIB, IIC, or III melanoma, use of laboratory tests and imaging tests such as CT, Patients with stage IV melanoma will have regular clinical, laboratory, and radiologic evalu- ations to mo Follow-Up After Treatment of Melanom
- 40. Treatment of Recurrent or Metastatic Dis Local recurrence is one which recurs within 5 cm radius of the primary tumour in skin or subcutaneous tis For Distant Spread: o Brain, lung and liver are the most common sites; skin, bone, GI are less common sites. But melano o Distant spread when found or suspected, CT scan of head, chest, abdomen and pelvis are needed. PET sc
- 42. In-transit Disease• In-transit recurrence represents endolymphatic disease manifested by cutaneous or subcutaneous tumor nodules between the primary tumour site and regional nodal basin. • Local injection of refractory in-transit disease with agents such as Bacille Calmette-Guérin (BCG), interferon, and interleukin-2 may, in some cases, result in complete response. • Laser and other ablative therapies may be considered. • When confined to the upper or lower extremity, may be treated by hyperthermic isolated limb perfusion (HILP) with L-phenylalanine mustard (melphalan). • Repeat perfusion can be performed in patients who recur, but should only be attempted in patients who responded well to the initial perfusion. • Percutaneous catheters are placed into the major artery and vein supplying the extremity, followed by pneumatic tourniquet isolation. Perfusion with ILI is accomplished by manual circulation using a syringe.
- 43. Examples of in-transit melanoma of the arm (left) and leg (right). Note the distribution and extent of disease, making these presentations very poor candidates for surgical excision. On the left, there is evidence of in-transit metastases both within the area of previous skin flap, as well as extending more proximally along its course of lymphatic drainage. On the right, there is extensive disease extending up to the inguinal crease.
- 44. Immunotherapy/Biological Therapy o It is done using specific tumour antibodies, BCG, levamisole, Corynebacterium parvum, alpha interf o Biochemotherapy is combination of CVD with interferon α and interleukin 2. o GM2 ganglioside based vaccine (stimulates production of IgM antibodies), Melacine (contains mela
- 45. Unknown Primary Melanoma Occurs in less than 2% of all melanoma cases and less than 5% of all patients who present with metastatic melanoma. Occult melanomas (primary unknown) are common in : — Anus — Scalp — External auditory canal — Nail bed — Genitalia — Eye — Adrenal medulla Melanoma During Pregnancy The prognosis is same patients treated during pregnancy is no different from non pregnant patients of a similar stage. Noncutaneous Melanomas the eye, mucosal surfaces, and unknown primary sites. MRI of the liver is a more sensitive test, which will often demonstrate hundreds of small metastases. The most common sites of origin for melanomas arising on the mucous membranes are the head and neck, anal canal, rectum, and female genitalia. Compared with melanomas arising on the skin, mucosal melanomas are more advanced and have a uniformly poor prognosis. these tumors should be excised to negative margins. Special Situations and Non-cutaneous Melanoma Ocular melanoma is the most common malignancy arising in the eye. Ocular melanoma rarely metastasizes to lymph nodes because the uveal tract has no lymphatic vessels. Ocular mela
- 47. Prevention Much excessive UV radiation exposure, in the form sunbathing and tanning bed use, is intentional and completely preventable. Recommendations for reducing UV radiation exposure include avoiding these activities, use of protective clothing, and use of sunscreens. Although most experts believe that the use of sun- screens will reduce the risk of melanoma, this topic is controversial, because some have suggested that sunscreens may provide a false sense of security and allow persons at risk to experience more prolonged sun exposure. However, a meta- analysis of 18 studies has found no evidence that use of sun- screens increased the incidence of melanoma.
- 48. Cutaneous squamous cell carcinoma/ Epithelioma/ Khangri Cancer) (Chimney Cancer/ Epidermoid carcinoma • SCC is a malignant tumour of keratinising cells of the epidermis or its appendages. It arises from the stratum germinatum of the epidermis and expresses cytokeratins 1 and 10. Epidemiology • SCC is the second most common form of skin cancer. • The time taken to develop an SCC after radiation exposure is proportional to the wavelength of the radiation. • SCC is also caused by chemical carcinogens (arsenicals, tar), and infection with human papilloma virus 5 and 16. • There is also evidence that current and previous tobacco use doubles the relative risk of SCC.Exposure to UV B rays (ultraviolet rays are A,B,C types) causes SCC by direct carcinogenic effects on keratinocytes, unrepaired mutations, decreased immune surveillance response, inhibition of tumour rejection, mutation of p53 suppressor gene (seen in 90% SCC).
- 49. It occurs in premalignant conditions like Bowen’s disease, Paget’s disease, leukoplakia, chronic scars, chemically induced chronic irritation, radiodermatitis, senile keratosis, e.g. Khangri cancer in Kashmir, Chimney scrotal cancer, Kang cancer of Tibetans. Bowen's disease, also known as squamous cell carcinoma in situ[ Extramammary Paget’s disease (EMPD)
- 50. Examination Squamous cell carcinoma ▪ Associated with chronic inflammation ▪ Invariably ulcerated lesion ▪ Metastasis in 2 per cent cases Common Sites are: o Dorsum of hand, limbs, face, and skin of abdominal wall SCC can occur in external genitalia, mucocutaneous junction, oral cavity, respiratory system, oesophagus, gall- bladder, in urinary bladder as metaplasia from transitional cell lining.
- 51. o An ulcerative or ulceroproliferative lesion. o Raised and everted edge. o Indurated base and edge. o Bloody discharge from the lesion. o Regional lymph nodes are commonly involved, which are hard, nodular, initially mobile but eventually f o Usually blood spread does not occur.
- 52. Variants o Marjolin’s ulcer which occurs in chronic scar is a type of squamous cell carcinoma without lymph node s no lymphatics in scar tissue, it will not spread to lymph nodes. o Verrucous carcinoma is a squamous cell carcinoma, commonly occurring in mucous membrane or muco
- 53. Histology An invasive, epidermal keratinising tumour characterised by proliferation of atypical squamous cells with ‘horn pearls’
- 54. o Radiotherapy using radiation needles,moulds,etc.isgiven. o Wide excision, 2 cm clearance followed by skin grafting or flaps. Reconstruction is usually done by primary split skin grafting (SSG/Thiersch). Delayed skin grafting also can be done once wound granulates well. Often flaps of different types may be needed depending on the site of lesion. o Amputation with one joint above. For lymph nodes, block dissection of the regional lymph nodes is done. o Curative radiotherapy (RT) is also useful in tumours which are not adherent to deeper planes or cartilage as SCC is radiosensitive. o In adv o Chemotherapy is given using methotrexate, vincristine, bleomycin. o Field therapy using cryo probe or topical fluorouracil or electrodessication. Treatment
- 58. In contrast to SCCs and actinic keratoses, there is no precursor skin lesion for BCCs. Basal cell carcinoma/ Rodent ulcer/ Tear cancer This tumour of low-grade malignancy is common in white-skinned people. It originates from th skin. It does not arise from mucosa. It is the commonest (70%) malignant skin tumour. o It is more common in white-skinned people than blacks. o Common in places where exposure to UV light is more (Australia).
- 59. ONGHREN’S LINE
- 60. Examination It starts as a small brownish-red nodule with translucent colour and shiny surface showing a net work of capillaries. At this stage it is diagnosed due to its hardness, painlessness and presence of capillaries. Later on the tumour becomes ulcerated with a well defined hard and raised edge (but not everted as seen in ^ epithelioma) with a beaded appearance. There is a central scab but the margin gradually spreads and infiltrates into the surrounding tissues as well as deeper tissues even up to the bone. This characteristic feature of eroding the tissues, which come in contact with it, has given it the name ‘rodent’. At first it may itch, but at a later stage it may be painful if it has eroded any nerve. Dissemination by lymphatic or blood vessels does not occur. So the regional lymph nodes are not enlarged and there will be no metastasis to the distant organs. There may be squamous celled carcinomatous change, though very rare.
- 61. 1. Nodular. 2. Cystic/nodulocystic. 3. Ulcerative. 4. Multiple,oftenassociatedwithsyndromesandothermalig- nancies. 5. Pigmented BCC—mimics melanoma. 6. Geographical or field fire or forest fire BCC is wide area involvement with central scabbing and peripheral active proliferating edge. 7. Basisquamous—behaves like squamous cell carcinoma Clinicopathological Types a. Superficial type—small buds of tumour masses. b. Morpheic type—dense stroma with basal cells and type IV collagen; spreads rapidly. c. Fibroepithelioma type of Pinkus shows elongated cords of basaloid cells with mesh work. Types
- 62. • Radiosensitive. • Radiotherapy is not given, if it erodes cartilage or bone. • RT is not given to BCC of ear and close to lacrimal canaliculi. Surgery: Wide excision (1 cm clearance) with skin grafting, primary suturing or flap (Z plasty, rhomboid flap, rotation flap) is the procedure of choice. Laser surgery. Cryosurgery. • MOHS (Microscopically Oriented Histographic Surgery) is useful to get a clearance margin and in conditions like BCC close to eyes, nose or ear, to preserve Treatment
- 63. MOHS (Microscopically Oriented Histographic Surgery)
- 66. Ninety-five per cent of local recurrence and regional metas- tases occur within five years, thus follow up b Prognosis is excellent if the appropriate method of treatment is used in early primary basal-cell c
- 67. Uncommon Cutaneous Malignancies Cutaneous angiosarcoma is a rare, aggressive, soft tissue sarcoma derived from blood or lymphatic vessel endothelium. Dermato brosarcoma protuberans is a low-grade sarcoma arising from dermal fibroblasts.
- 68. Extramammary Paget’s disease (EMPD) Kaposi’s sarcoma Merkel cell carcinoma
- 70. “Destructive treatment options are generally reserved for low-risk basal cell tumors and use a variety of methods to destroy neoplastic tissue including electrosurgery, cryosurgery, topical 5-fluorouracil, topical imiquimod, intralesional interferon, radiation, and photodynamic therapy. ”
- 71. Primary closure
- 72. Skin grafting
- 73. Tissue expander
- 74. Local flap
- 75. Local flap
- 76. Local flap
- 77. Free flap
- 78. Free flap
- 79. Conclusion The important principles in the management of these entities are the same as those reviewed earlier: 1. Clinicians must have a low threshold for biopsy of new or changing skin lesions. 2. The diagnosis is made by biopsy and histologic analysis. 3. If appropriate, surgical excision is performed, with histo- logically de ned negative margins. 4. Further treatment and follow-up schedules will be deter- mined by the speci c diagnosis.
- 80. Any questions?
- 81. Bibliography ❖ Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 19th Edition ❖ Bailey & Love's Short Practice of Surgery 26E ❖ https://www.nccn.org ❖ Grabb & Smith's Plastic Surgery ❖ Das’ manual of clinical surgery
