Quality indicators for prevention and management of pressure ulcers
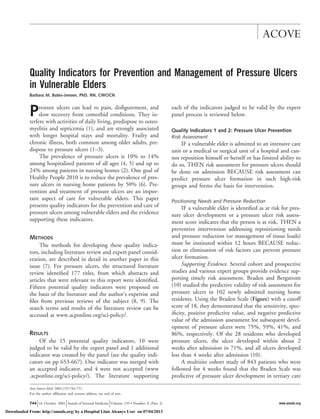
- 1. Quality Indicators for Prevention and Management of Pressure Ulcers in Vulnerable Elders Barbara M. Bates-Jensen, PhD, RN, CWOCN Pressure ulcers can lead to pain, disfigurement, and slow recovery from comorbid conditions. They in-terfere with activities of daily living, predispose to osteo-myelitis and septicemia (1), and are strongly associated with longer hospital stays and mortality. Frailty and chronic illness, both common among older adults, pre-dispose to pressure ulcers (1–3). The prevalence of pressure ulcers is 10% to 14% among hospitalized patients of all ages (4, 5) and up to 24% among patients in nursing homes (2). One goal of Healthy People 2010 is to reduce the prevalence of pres-sure ulcers in nursing home patients by 50% (6). Pre-vention and treatment of pressure ulcers are an impor-tant aspect of care for vulnerable elders. This paper presents quality indicators for the prevention and care of pressure ulcers among vulnerable elders and the evidence supporting these indicators. METHODS The methods for developing these quality indica-tors, including literature review and expert panel consid-eration, are described in detail in another paper in this issue (7). For pressure ulcers, the structured literature review identified 177 titles, from which abstracts and articles that were relevant to this report were identified. Fifteen potential quality indicators were proposed on the basis of the literature and the author’s expertise and files from previous reviews of the subject (8, 9). The search terms and results of the literature review can be accessed at www.acponline.org/sci-policy/. RESULTS Of the 15 potential quality indicators, 10 were judged to be valid by the expert panel and 1 additional indicator was created by the panel (see the quality indi-cators on pp 653-667). One indicator was merged with an accepted indicator, and 4 were not accepted (www .acponline.org/sci-policy/). The literature supporting each of the indicators judged to be valid by the expert panel process is reviewed below. Quality Indicators 1 and 2: Pressure Ulcer Prevention Risk Assessment IF a vulnerable elder is admitted to an intensive care unit or a medical or surgical unit of a hospital and can-not reposition himself or herself or has limited ability to do so, THEN risk assessment for pressure ulcers should be done on admission BECAUSE risk assessment can predict pressure ulcer formation in such high-risk groups and forms the basis for intervention. Positioning Needs and Pressure Reduction IF a vulnerable elder is identified as at risk for pres-sure ulcer development or a pressure ulcer risk assess-ment score indicates that the person is at risk, THEN a preventive intervention addressing repositioning needs and pressure reduction (or management of tissue loads) must be instituted within 12 hours BECAUSE reduc-tion or elimination of risk factors can prevent pressure ulcer formation. Supporting Evidence. Several cohort and prospective studies and various expert groups provide evidence sup-porting timely risk assessment. Braden and Bergstrom (10) studied the predictive validity of risk assessment for pressure ulcers in 102 newly admitted nursing home residents. Using the Braden Scale (Figure) with a cutoff score of 18, they demonstrated that the sensitivity, spec-ificity, positive predictive value, and negative predictive value of the admission assessment for subsequent devel-opment of pressure ulcers were 75%, 59%, 41%, and 86%, respectively. Of the 28 residents who developed pressure ulcers, the ulcer developed within about 2 weeks after admission in 71%, and all ulcers developed less than 4 weeks after admission (10). A multisite cohort study of 843 patients who were followed for 4 weeks found that the Braden Scale was predictive of pressure ulcer development in tertiary care Ann Intern Med. 2001;135:744-751. For the author affiliation and current address, see end of text. ACOVE 744 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) www.annals.org Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 2. centers, Veterans Affairs medical centers, and skilled nursing facilities (11). As part of the study, prescription of preventive interventions for turning and pressure re-duction were evaluated in all three health care settings. Regardless of setting, turning schedules and pressure re-duction were prescribed less frequently (7.7% and 34%) for patients at no risk or low risk (Braden Scale scores $ 16) than for patients at moderate or high risk (Braden Scale scores # 15; 51% and 69%) (12). In another pro-spective cohort study of 200 newly admitted nursing home residents, the best predictor of all stages of pres-sure ulcer formation was Braden Scale score (13). Other investigators also found an association between preven-tive interventions and Braden Scale scores, in particular the subscale scores for mobility, friction, and shear (14). Prevention interventions are ordered and seem to be used more frequently for people with high-risk Braden Scale scores. However, data showing the effectiveness of the interventions themselves are lacking. Various expert groups, including the National Pressure Ulcer Advisory Panel (NPUAP) (15), the Agency for Health Care Pol-icy and Research (AHCPR) Panel for Prevention and Figure. The Braden Scale for predicting risk for pressure ulcers. Quality Indicators for Pressure Ulcers ACOVE www.annals.org 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) 745 Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 3. Prediction of Pressure Ulcers (2), and the American Medical Directors Association (AMDA) (3) recommend performing risk assessment in persons who cannot repo-sition themselves or have limited ability to do so. Quality Indicator 3: Pressure Ulcer Prevention Nutrition IF a vulnerable elder is identified as at risk for pres-sure ulcer development and has malnutrition (involun-tary weight loss of $10% over 1 year or low albumin or prealbumin levels), THEN nutritional intervention or dietary consultation should be instituted BECAUSE poor diet, particularly low dietary protein intake, is an independent predictor of pressure ulcer development. Supporting Evidence. Studies have shown a relation-ship between risk factors for malnutrition, such as invol-untary weight loss, anorexia, gastrointestinal illnesses, cancer, low caloric intake, and low albumin level and pressure ulcer formation; some studies have found a re-lationship between ulcer severity and severity of malnu-trition (16 –18). Furthermore, several studies have shown associations between low serum albumin level and the presence (19, 20), severity (17, 18), and healing (21, 22) of pressure ulcers. Other measures of nutri-tional status, such as body weight, have been shown to correlate with presence (19, 20) and severity (17) of pressure ulcers. Although no direct evidence shows that adequate nutrition will prevent ulcers, these studies pro-vide indirect evidence that prevention of malnutrition will reduce risk for pressure ulcer formation. Quality Indicator 4 Pressure Ulcer Evaluation IF a vulnerable elder presents with a pressure ulcer, THEN the pressure ulcer should be assessed for loca-tion, depth and stage, size, and presence of necrotic tis-sue BECAUSE baseline assessment guides interventions, provides data for later comparison to evaluate healing, and can help predict time to healing. Supporting Evidence. No controlled trials of assess-ment of pressure ulcers have been done, and some ex-perts believe that such studies may be impractical or irrelevant (23). Several sets of guidelines support formal assessment of pressure ulcers, with documentation of findings, and focus on wound characteristics as a useful method for evaluating and documenting healing. The NPUAP suggested that 1) assessment should include multiple characteristics; 2) pressure ulcer staging is use-ful for diagnostic purposes only; and 3) size and stage are insufficient measures of healing and, although im-portant, should be used in conjunction with assessment of other wound characteristics (24). Others have also acknowledged the role of assessment in planning and evaluating therapy (3, 25, 26). Observational data support these consensus state-ments and suggest that many wound characteristics are important predictors of healing or determinants of in-terventions. Wound Depth and Stage Pressure ulcers are commonly classified according to staging systems based on the depth of tissue destruction. Stage 1 lesions are least severe, and stage 4 are most severe. Staging systems are best used to diagnose wound severity and show a relationship to healing outcomes, but they do not facilitate monitoring of healing over time (2, 24, 26, 27). Full-thickness wounds (stage 3 and stage 4) generally take longer to heal than partial-thick-ness wounds (stage 2) (28). A prospective study showed that stage 2 pressure ulcers were 5.2 times more likely to heal than stage 4 pressure ulcers (29). Several other pro-spective studies also found that wound depth was a pre-dictor of healing and time to healing (21, 30). Two retrospective studies demonstrated that wound depth was related to healing characteristics (31) and that change in depth was related to healing time (8), yet both studies found that initial wound depth did not correlate with healing. Size Several studies have demonstrated a relationship be-tween wound surface area and time to complete healing. In a prospective study to determine progress of healing within specific time frames, van Rijswijk (32) examined the characteristics of full-thickness pressure ulcers in 119 patients (48 of whom had full-thickness ulcers) who were seen in diverse settings. Healing was measured by using surface area tracings, with follow-up of 15 months. Mean reduction in wound surface area for ul-cers that healed versus those that did not was significant at 2 weeks (45% vs. 23%) and at 4 weeks (77% vs. 18%). In a secondary analysis of full-thickness pressure ACOVE Quality Indicators for Pressure Ulcers 746 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) www.annals.org Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 4. ulcers, only 25% healed completely within 50 days, but three quarters had 50% reduction in surface area within 39 days (33). Ulcers with a surface area decrease of at least 39% after 2 weeks healed more quickly than those with a lesser decrease in surface area (median time to healing, 53 vs. 70 days). Retrospective studies also sup-port the relationship between early reduction in surface area and shorter time to healing (8, 31). Presence of Necrotic Tissue Wound bed characteristics determine treatment op-tions (8, 34). Several studies have shown that replace-ment of necrotic tissue with granulation and epithelial tissue is indicative of healing (32), and the presence of necrotic tissue at baseline is associated with slower heal-ing (35). Other Characteristics and Assessment Tools Results of studies of other wound characteristics, such as exudate and undermining, in relation to healing time have been inconclusive (8, 21, 33–36). Nonethe-less, assessment is recommended because it can guide treatment (8). Use of a standardized instrument or tool for assess-ment and documentation of pressure ulcers, such as the Pressure Sore Status Tool (37) or the Pressure Ulcer Scale for Healing (36), is suggested, but no study has examined the effect of standardized evaluation and doc-umentation on pressure ulcer outcomes. Quality Indicators 5 and 6 Management of Full-Thickness Pressure Ulcers IF a vulnerable elder presents with a clean full-thickness pressure ulcer and has no improvement after 4 weeks of treatment, THEN the appropriateness of the treatment plan and the presence of cellulitis or osteomy-elitis should be assessed BECAUSE clean full-thickness pressure ulcers should show evidence of healing or im-provement within 4 weeks and lack of improvement should stimulate a change in approach. Management of Partial-Thickness Pressure Ulcers IF a vulnerable elder presents with a partial-thick-ness pressure ulcer and has no improvement after 2 weeks of treatment, THEN the appropriateness of the treatment plan should be assessed BECAUSE partial-thickness Quality Indicators for Pressure Ulcers ACOVE pressure ulcers should show evidence of heal-ing or improvement within 2 weeks and lack of im-provement should stimulate a change in approach. Supporting Evidence. No direct evidence indicates that reassessment of nonhealing ulcers will improve out-comes. However, it is logical that reassessment is a nec-essary first step to identify causes of and, hence, treat nonhealing ulcers. These two quality indicators are supported by evi-dence on rate of healing and healing outcomes from several studies. A randomized, controlled trial involving 85 patients found that up to 42% of stage 2 ulcers healed within 30 days and 75% healed within 60 days, whereas only 17% of stage 3 and 4 ulcers healed within 60 days (30). Similar outcomes were noted in a prospec-tive cohort study of 89 nursing home residents with stage 2 or greater pressure ulcers. After 6 weeks of follow-up, 65% of stage 2 ulcers, 14% of stage 3 ulcers, and no stage 4 ulcers healed (29). In Brandeis and col-leagues’ (28) cohort study of 1626 patients with a stage 2 or greater pressure ulcer who were admitted to 1 of 51 nursing, up to 54% of stage 2 ulcers healed in 3 months and 74% healed in 6 months (28). Healing rates for stage 3 and 4 ulcers were slower; 31% and 23% healed in 3 months and 59% and 33% healed in 6 months, respectively. Data from a randomized, controlled trial (35) indicated much faster healing times for stage 2 ul-cers and provide primary support for the 2-week time frame for the partial-thickness quality indicator: The median healing time was 9 to 11 days, and three quar-ters of the ulcers healed within 14 to 26 days, depending on topical treatment. In a retrospective study of 143 pressure ulcers, change in surface area at 1 week was a strong predictor of time to 50% healing. The median time to 50% heal-ing among ulcers at all stages that had decreased surface area within 1 week was 21 to 26 days; in contrast, wounds with no change in surface area reached 50% healing in a median of 34 days (8), and an increase in surface area at 1 week was predictive of nonhealing. Reported mean or median times to healing are 8.7 to 38 days (22, 30, 35) for partial-thickness stage 2 ulcers; full-thickness stage 3 or 4 ulcers will heal after 8 to 10 weeks of therapy in 10% to 40% of patients (28, 32). Some investigators have shown that the percentage reduction in surface area after 1, 2, or 4 weeks of treat-ment is predictive of time to healing (8, 33). The basis www.annals.org 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) 747 Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 5. for the 4-week timeframe in the full-thickness quality indicator is primarily supported by van Rijswijk and Polansky’s study of full-thickness pressure ulcers and percentage reduction in surface area as predictors of time to healing (33). Quality Indicator 7 Pressure Ulcer Debridement IF a vulnerable elder presents with a full-thickness sacral or trochanteric pressure ulcer covered with ne-crotic debris or eschar, THEN debridement by using sharp, mechanical, enzymatic, or autolytic procedures should be done within 3 days of diagnosis BECAUSE dead tissue is a physical obstacle to healing tissue and provides a medium for bacterial invasion and prolifera-tion, which places the patient at high risk for wound infection. Supporting Evidence. Wound debridement can be performed by using sharp, mechanical, enzymatic, or autolytic methods. Sharp debridement involves use of a scalpel, scissors, or other sharp instrument to remove nonviable tissue. One multicenter trial of the effects of a topical growth factor versus placebo on wound healing in 118 patients noted incidentally that sharp debride-ment was positively associated with healing of diabetic ulcers (38). In this study, all patients received sharp de-bridement initially and then as needed throughout 20 weeks of follow up. In post hoc analysis, centers that used sharp debridement more frequently (debridement at up to 87% of visits) produced better healing rates (up to 83%) than did centers that used sharp debridement less often (debridement at 15% to 43% of visits; up to 64% healed). Sharp debridement can be safely per-formed in a fairly aggressive manner at the bedside in a sequential fashion (daily or every other day) by various health care providers. Attention to patient comfort is recommended (systemic or topical analgesia), and some have suggested benefits to combining bedside sequential sharp debridement with other forms of debridement to maximize response (39). Mechanical debridement involves the use of wet-to-dry dressings, whirlpool, or lavage or wound irrigation. The AHCPR panel recommended cautious use of mechanical wet-to-dry dressings for debridement be-cause removal of dressing may cause trauma to new granulation and epithelial tissue. Because debridement with wet-to-dry dressings is painful, the AHCPR panel recommends pain management, such as administration of a systemic analgesic before dressing removal (25). Coarsely woven gauze or cotton sponges appear to be more effective than finer materials in mechanical de-bridement (40). Enzymatic debridement involves applying a concen-trated, commercially prepared enzyme to the surface of the necrotic tissue, with the expectation that it will ag-gressively degrade necrosis by digesting devitalized tis-sue. A randomized, controlled trial of enzymatic de-bridement for necrotic wounds reported a mean time of 8 days to debride stage 4 pressure ulcers with an amor-phous hydrogel dressing and a mean time of 12 days for debridement with an enzymatic preparation containing streptokinase and streptodornase (41). These times did not differ significantly, suggesting that an agent with enzyme activity was unnecessary. Autolytic debridement is use of the body’s own mechanisms to remove nonviable tissue. Maintaining a moist wound environment allows collection of fluid at the wound site, which allows enzymes within the wound to digest necrotic tissue. Autolytic debridement, which typically involves adequate wound cleansing to wash out partially degraded nonviable tissue, is more effective than wet-to-dry gauze dressings because it removes only necrotic tissue and therefore protects healthy tissues (42– 44). Mulder and colleagues (42) evaluated 16 pa-tients in a randomized, controlled trial of a hypertonic hydrogel versus wet-to-dry gauze for wound debride-ment (the hypertonicity of the gel assists with autolytic debridement by pulling fluid into the area through os-motic forces) (42). The results suggested that the hydro-gel could safely facilitate removal of dry adherent eschar from wounds. Other investigators also have found amorphous hydrogels to be effective in removing ne-crotic debris from wounds (43– 45). Quality Indicator 8 Pressure Ulcer Management: Cleansing IF a vulnerable elder has a stage 2 or greater pressure ulcer, THEN a topical antiseptic should not be used on the wound BECAUSE topical antiseptics may harm the healthy wound bed. Supporting Evidence. No controlled trials have exam-ined the effectiveness or safety of wound cleansing. Con-traindications to the use of antiseptic and antimicrobial ACOVE Quality Indicators for Pressure Ulcers 748 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) www.annals.org Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 6. solutions for cleansing clean pressure ulcers are based on several laboratory studies (46–49). Two studies tested antimicrobial wound cleansers and solutions for toxicity to polymorphonuclear leukocytes. Results showed that even serial dilutions of the products diminished the vi-ability and function of polymorphonuclear leukocytes; in contrast, nonantimicrobial solutions did not cause substantial toxicity to polymorphonuclear leukocytes (46, 47). On the basis of early animal model studies (48, 49), the AHCPR guidelines recommend normal saline as the preferred cleanser because it is noncytotoxic (25). Quality Indicators 9 and 10 Pressure Ulcer Debridement for Systemic Infection IF a vulnerable elder with a full-thickness pressure ulcer presents with systemic signs and symptoms of in-fection, such as elevated temperature, leukocytosis, con-fusion, and agitation, and these signs and symptoms do not have another identified cause, THEN the ulcer should be debrided of necrotic tissue within 12 hours BECAUSE debridement will reduce dead tissue that provides a medium for bacterial invasion and may lead to systemic infection. Pressure Ulcer Culture for Systemic Infection IF a vulnerable elder with a full-thickness pressure ulcer presents with systemic signs and symptoms of in-fection, such as elevated temperature, leukocytosis, con-fusion, and agitation, and these signs and symptoms do not have another identified cause, THEN a tissue biopsy or needle aspiration sample should be obtained and sent for culture and sensitivity testing within 12 hours BECAUSE high bacterial burdens inhibit wound heal-ing and may lead to systemic infection, and needle as-piration or tissue biopsy is the best indicator of bacterial invasion into tissue. Supporting Evidence. Wound infection extends the inflammatory phase of healing, delays collagen synthesis, retards epithelialization, and causes more injury to the tissues because the bacteria produce toxic by-products and compete with fibroblasts and other cells for limited amounts of oxygen and nutrients (50, 51). Signs and symptoms of systemic infection may be due to spread from a full-thickness pressure ulcer. To treat the infection, the source of the infection must be identified; impediments to healing must be removed; and, if possible, the organism causing the infection must be identified. Standard swab cultures do not aid in di-agnosis of infection in pressure ulcers because they de-tect only surface contaminants and not the organism that caused the tissue infection (52). The AHCPR pres-sure ulcer treatment guidelines recommend wound cul-ture of a tissue biopsy or needle aspiration sample when infection is suspected (25). This procedure may be im-practical at some centers, and the NPUAP supports use of a specialized swab technique to culture pressure ulcer wound beds (24, 53). The recommended method of quantitative swab culture involves cleansing the wound with solution that contains no antiseptic. The end of a sterile cotton-tipped applicator is rotated in a 1-cm2 area of the wound for 5 seconds (53, 54) with enough pres-sure to cause tissue fluid to be absorbed in the cotton tip of the swab. The swab tip is inserted in the tube con-taining transport media and is sent to the laboratory. Swab culture was not included in the indicator because of the difficulty in distinguishing technique from the medical record. Tissue biopsy is removal of a piece of tissue by using a scalpel or a punch biopsy instrument. The area may be treated with topical anesthetic or injected with local an-esthetic. The biopsy is performed, pressure is applied to the area to control bleeding, and the tissue is sent to the laboratory. Needle aspiration involves insertion of a 22- gauge needle (attached to a 10-mL disposable syringe with 0.5 mL of air in the syringe) through intact skin next to the wound. Suction is achieved by briskly with-drawing the plunger to the 10-mL mark. The needle is moved backward and forward at different angles for two to four explorations. The plunger is gently returned to the 0.5-mL mark, the needle is withdrawn and capped, and the specimen is sent to the laboratory. In the setting of possible systemic infection, the full-thickness ulcer should be treated to decrease the likeli-hood that it is a source of hematogenous bacterial seeding. This is particularly true for wounds with foul-smelling drainage that are generally infected or filled with ne-crotic debris. For such ulcers, healing time is prolonged because tissue destruction may be progressive (55). De-bridement of the wound, with special attention to areas of undermining or tunneling, removes dead tissue that provides a medium for bacterial growth and invasion. Because systemic infection is life-threatening, debride-ment of the wound bed should be done within 12 hours. Quality Indicators for Pressure Ulcers ACOVE www.annals.org 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) 749 Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 7. Quality Indicator 11 Topical Dressings IF a vulnerable elder presents with a clean full-thickness or a partial-thickness pressure ulcer, THEN a moist wound-healing environment should be provided with topical dressings BECAUSE wounds heal better in a moist environment. Supporting Evidence. Several investigators have com-pared a moist environment with dry dressings for wound healing. All have noted faster healing with moist wound dressings than with wet-to-dry saline gauze dressings (22, 56, 57). The AHCPR guidelines on pres-sure ulcer treatment (25), which are supported by the American Medical Directors Association (3) and NPUAP (24), also advocate the use of moist dressings over dry dressings. DISCUSSION Despite an increase in pressure ulcer research since the publication of the AHCPR guidelines on pressure ulcers, few quality indicators are supported by substan-tial evidence. Through a literature search and synthesis coupled with a two-stage expert panel process, 11 valid quality indicators for pressure ulcers were identified. These indicators span pressure ulcer care from preven-tion and assessment to topical treatments. Although they are not comprehensive, they provide a baseline for measures that may discriminate between quality and substandard care. From University of California, Los Angeles, Los Angeles, California; and the Borun Center for Gerontological Research, Los Angeles, California. Grant Support: By a contract from Pfizer Inc. to RAND. Acknowledgments: The author thanks Dan Osterweil, MD, for review of an earlier version of the paper containing the full set of proposed quality indicators, and Patricia Smith for technical assistance. Requests for Single Reprints: Barbara Bates-Jensen PhD, RN, CWOCN, UCLA Borun Center for Gerontological Research, 7150 Tampa Avenue, Reseda, CA 91335. References 1. Thomas DR. Pressure ulcers. In: Cassel CK, Cohen HJ, Larson EB, Meier DE, Resnick NM, Rubenstein LZ, et al, eds. Geriatric Medicine. 3rd ed. New York: Springer; 1997:767-85. 2. Pressure Ulcers in Adults: Prediction and Prevention. Clinical Practice Guide-line, Number 3. Rockville, MD: U.S. Department of Health and Human Ser-vices, Public Health Service, Agency for Health Care Policy and Research; 1992. AHCPR publication no. 92-0047. 3. Pressure Ulcers: Clinical Practice Guideline. Columbia, MD: American Med-ical Directors Association; 1996. 4. Whittington K, Patrick M, Roberts JL. A national study of pressure ulcer prevalence and incidence in acute care hospitals. J Wound Ostomy Continence Nurs. 2000;27:209-15. [PMID: 10896746] 5. Amlung S, Miller W, Bosley LM, Runfola A, Barnett R. National prevalence pressure ulcer survey: a benchmarking approach [Abstract]. In: 14th Annual Clin-ical Symposium on Wound Care. The Quest for Quality Wound Care: Solutions for Clinical Practice. Denver, Colorado, 30 September–4 October 1999. Spring-house, PA: Springhouse Corp.; 2000:234. 6. Objective 1-16. In: Healthy People 2010. Washington, DC: U.S. Department of Health and Human Services; 2000. 7. Shekelle PG, MacLean CH, Morton SC, Wenger NS. Assessing care of vulnerable elders: methods for developing quality indicators. Ann Intern Med. 2001;135:647-52. 8. Bates-Jensen BM. A quantitative analysis of wound characteristics as early predictors of healing in pressures sores [Abstract]. Dissertation Abstracts Inter-national, Volume 59, Number 11. Los Angeles: University of California, Los Angeles; 1999. 9. Bates-Jensen BM. Pressure ulcers: pathophysiology and prevention. In: Suss-man C, Bates-Jensen BM, eds. Wound Care: A Collaborative Practice Manual for Physical Therapists and Nurses. Gaithersburg, MD: Aspen Publishers; 1998:235-70. 10. Braden BJ, Bergstrom N. Predictive validity of the Braden Scale for pressure sore risk in a nursing home population. Res Nurs Health. 1994;17:459-70. [PMID: 7972924] 11. Bergstrom N, Braden B, Kemp M, Champagne M, Ruby E. Predicting pressure ulcer risk: a multisite study of the predictive validity of the Braden Scale. Nurs Res. 1998;47:261-9. [PMID: 9766454] 12. Bergstrom N, Braden B, Kemp M, Champagne M, Ruby E. Multi-site study of incidence of pressure ulcers and the relationship between risk level, demographic characteristics, diagnoses, and prescription of preventive interven-tions. J Am Geriatr Soc. 1996;44:22-30. [PMID: 8537586] 13. Bergstrom N, Braden B. A prospective study of pressure sore risk among institutionalized elderly. J Am Geriatr Soc. 1992;40:747-58. [PMID: 1634717] 14. Xakellis GC, Frantz RA, Arteaga M, Nguyen M, Lewis A. A comparison of patient risk for pressure ulcer development with nursing use of preventive inter-ventions. J Am Geriatr Soc. 1992;40:1250-4. [PMID: 1447443] 15. Statement on Pressure Ulcer Prevention. Reston, VA: National Pressure Ulcer Advisory Panel; 1992. Available at www.npuap.org/positn1.htm. Accessed 29 May 2001. 16. Thomas DR. The role of nutrition in prevention and healing of pressure ulcers. Clin Geriatr Med. 1997;13:497-511. [PMID: 9227941] 17. Moolten SE. Bedsores in the chronically ill patient. Arch Phys Med Rehabil. 1972;53:430-8. [PMID: 5077819] 18. Pinchcofsky-Devin GD, Kaminski MV Jr. Correlation of pressure sores and nutritional status. J Am Geriatr Soc. 1986;34:435-40. [PMID: 3084610] 19. Allman RM, Laprade CA, Noel LB, Walker JM, Moorer CA, Dear MR, et al. Pressure sores among hospitalized patients. Ann Intern Med. 1986;105: 337-42. [PMID: 3740674] 20. Berlowitz DR, Wilking SV. Risk factors for pressure sores. A comparison of cross-sectional and cohort-derived data. J Am Geriatr Soc. 1989;37:1043-50. [PMID: 2809051] 21. Allman RM, Walker JM, Hart MK, Laprade CA, Noel LB, Smith CR. Air-fluidized beds or conventional therapy for pressure sores. A randomized trial. Ann Intern Med. 1987;107:641-8. [PMID: 3310792] ACOVE Quality Indicators for Pressure Ulcers 750 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) www.annals.org Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
- 8. 22. Gorse GJ, Messner RL. Improved pressure sore healing with hydrocolloid dressings. Arch Dermatol. 1987;123:766-71. [PMID: 3555355] 23. van Rijswijk L, Braden BJ. Pressure ulcer patient and wound assessment: an AHCPR clinical practice guideline update. Ostomy Wound Manage. 1999;45: 56S-67S. [PMID: 10085976] 24. Description of NPUAP. National Pressure Ulcer Advisory Panel. Adv Wound Care. 1995;8(Suppl):93-5. [PMID: 7627416] 25. Treatment of Pressure Ulcers Guideline Panel. Treatment of Pressure Ulcers. Clinical Practice Guidelines, No.15. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service, Agency for Health Care Policy and Research; 1994. AHCPR publication no. 95-0652. 26. Lazarus GS, Cooper DM, Knighton DR, Margolis DJ, Pecoraro RE, Rodeheaver G, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol. 1994;130:489-93. [PMID: 8166487] 27. NPUAP Statement on Reverse Staging of Pressure Ulcers. NPUAP Report: A Newsletter from the National Pressure Ulcer Advisory Panel. 1995;4:1-2. Available at www.npuap.org. Accessed 29 May 2001. 28. Brandeis GH, Morris JN, Nash DJ, Lipsitz LA. The epidemiology and natural history of pressure ulcers in elderly nursing home residents. JAMA. 1990; 264:2905-9. [PMID: 2232085] 29. Berlowitz DR, Wilking SV. The short-term outcome of pressure sores. J Am Geriatr Soc. 1990;38:748-52. [PMID: 2370394] 30. Ferrell BA, Osterweil D, Christenson P. A randomized trial of low-air-loss beds for treatment of pressure ulcers. JAMA. 1993;269:494-7. [PMID: 8338511] 31. Bates-Jensen BM. The Pressure Sore Status Tool a few thousand assessments later. Adv Wound Care. 1997;10:65-73. [PMID: 9362584] 32. van Rijswijk L. Full-thickness pressure ulcers: patient and wound healing characteristics. Decubitus. 1993;6:16-21. [PMID: 8427640] 33. van Rijswijk L, Polansky M. Predictors of time to healing deep pressure ulcers. Ostomy Wound Manage. 1994;40:40-2, 44, 46-8 passim. [PMID: 7546099] 34. Van Rijswijk L. Wound assessment and documentation. In: Krasner D, Kane D, eds. Chronic Wound Care: A Compendium for Health Care Professionals. 2nd ed. Wayne, PA: Health Management Publications; 1997. 35. Xakellis GC, Chrischilles EA. Hydrocolloid versus saline-gauze dressings in treating pressure ulcers: a cost-effectiveness analysis. Arch Phys Med Rehabil. 1992;73:463-9. [PMID: 1580775] 36. Thomas DR, Rodeheaver GT, Bartolucci AA, Franz RA, Sussman C, Ferrell BA, et al. Pressure ulcer scale for healing: derivation and validation of the PUSH tool. The PUSH Task Force. Adv Wound Care. 1997;10:96-101. [PMID: 9362591] 37. Bates-Jensen BM, Vredevoe DL, Brecht ML. Validity and reliability of the Pressure Sore Status Tool. Decubitus. 1992;5:20-8. [PMID: 1489512] 38. Steed DL, Donohoe D, Webster MW, Lindsley L. Effect of extensive de-bridement and treatment on the healing of diabetic foot ulcers. Diabetic Ulcer Study Group. J Am Coll Surg. 1996;183:61-4. [PMID: 8673309] 39. Bates-Jensen BM. Management of necrotic tissue. In: Sussman C, Bates- Quality Indicators for Pressure Ulcers ACOVE Jensen BM, eds. Wound Care: A Collaborative Practice Manual for Physical Therapists and Nurses. Gaithersburg, MD: Aspen Publishers; 1999:139-58. 40. Mulder GD. Evaluation of three nonwoven sponges in the debridement of chronic wounds. Ostomy Wound Manage. 1995;41:62-4, 66-7. [PMID: 7546116] 41. Martin SJ, Corrado OJ, Kay EA. Enzymatic debridement for necrotic wounds. J Wound Care. 1996;5:310-1. [PMID: 8954418] 42. Mulder GD, Romanko KP, Sealey J, Andrews K. Controlled randomized study of a hypertonic gel for the debridement of dry eschar in chronic wounds. Wounds. 1993;5:112-5. 43. Flanagan M. The efficacy of a hydrogel in the treatment of wounds with non-viable tissue. J Wound Care. 1995;4:264-7. [PMID: 7614271] 44. Bale S, Banks V, Haglestein S, Harding KG. A comparison of two amor-phous hydrogels in the debridement of pressure sores. J Wound Care. 1998;7: 65-8. [PMID: 9543975] 45. Colin D, Kurring PA, Yvon C. Managing sloughy pressure sores. J Wound Care. 1996;5:444-6. [PMID: 9117814] 46. Foresman PA, Payne DS, Becker D, Lewis D, Rodeheaver GT. A relative toxicity index for wound cleansers. Wounds. 1993;5:226-31. 47. Hellewell TB, Major DA, Foresman PA, Rodeheaver GT. A cytotoxicity evaluation of antimicrobial and non-antimicrobial wound cleansers. Wounds. 1997;9:15-20. 48. Lineaweaver W, Howard R, Soucy D, McMorris S, Freeman J, Crain C, et al. Topical antimicrobial toxicity. Arch Surg. 1985;120:267-70. [PMID: 3970664] 49. Brennan SS, Leaper DJ. The effect of antiseptics on the healing wound: a study using the rabbit ear chamber. Br J Surg. 1985;72:780-2. [PMID: 4041708] 50. Robson MC. Disturbances of wound healing. Ann Emerg Med. 1988;17: 1274-8. [PMID: 3057944] 51. Robson MC, Stenberg BD, Heggers JP. Wound healing alterations caused by infection. Clin Plast Surg. 1990;17:485-92. [PMID: 2199139] 52. Rousseau P. Pressure ulcers in an aging society. Wounds. 1989;1:135-41. 53. Stotts NA. Determination of bacterial burden in wounds. Adv Wound Care. 1995;8(Suppl):46-52. [PMID: 7627404] 54. Levine NS, Lindberg RB, Mason AD Jr, Pruitt BA Jr. The quantitative swab culture and smear: a quick, simple method for determining the number of viable aerobic bacteria on open wounds. J Trauma. 1976;16:89-94. [PMID: 1255833] 55. Sapico FL, Ginunas VJ, Thornhill-Joynes M, Canawati HN, Capen DA, Klein NE, et al. Quantitative microbiology of pressure sores in different stages of healing. Diagn Microbiol Infect Dis. 1986;5:31-8. [PMID: 3709093] 56. Saydak SJ. A pilot test of two methods for the treatment of pressure ulcers. J Enterostomal Ther. 1990;17:139-42. [PMID: 2347993] 57. Sebern MD. Pressure ulcer management in home health care: efficacy and cost effectiveness of moisture vapor permeable dressing. Arch Phys Med Rehabil. 1986;67:726-9. [PMID: 3533007] www.annals.org 16 October 2001 Annals of Internal Medicine Volume 135 • Number 8 (Part 2) 751 Downloaded From: http://annals.org/ by a Hospital Lluis Alcanys User on 07/04/2013
