Health promotion
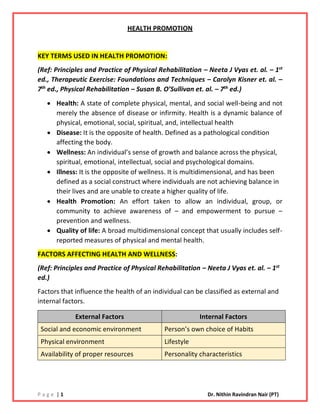
- 1. P a g e | 1 Dr. Nithin Ravindran Nair (PT) HEALTH PROMOTION KEY TERMS USED IN HEALTH PROMOTION: (Ref: Principles and Practice of Physical Rehabilitation – Neeta J Vyas et. al. – 1st ed., Therapeutic Exercise: Foundations and Techniques – Carolyn Kisner et. al. – 7th ed., Physical Rehabilitation – Susan B. O’Sullivan et. al. – 7th ed.) • Health: A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. Health is a dynamic balance of physical, emotional, social, spiritual, and, intellectual health • Disease: It is the opposite of health. Defined as a pathological condition affecting the body. • Wellness: An individual’s sense of growth and balance across the physical, spiritual, emotional, intellectual, social and psychological domains. • Illness: It is the opposite of wellness. It is multidimensional, and has been defined as a social construct where individuals are not achieving balance in their lives and are unable to create a higher quality of life. • Health Promotion: An effort taken to allow an individual, group, or community to achieve awareness of – and empowerment to pursue – prevention and wellness. • Quality of life: A broad multidimensional concept that usually includes self- reported measures of physical and mental health. FACTORS AFFECTING HEALTH AND WELLNESS: (Ref: Principles and Practice of Physical Rehabilitation – Neeta J Vyas et. al. – 1st ed.) Factors that influence the health of an individual can be classified as external and internal factors. External Factors Internal Factors Social and economic environment Person’s own choice of Habits Physical environment Lifestyle Availability of proper resources Personality characteristics
- 2. P a g e | 2 Dr. Nithin Ravindran Nair (PT) HEALTHY PEOPLE 2030: ▪ Overseen by the Office of Disease Prevention and Health Promotion in the Department of Health and Human Services. ▪ Vision 2030: A society in which all people can achieve their full potential for health and well-being across the lifespan. ▪ Overarching Goals: - o Attain healthy, thriving lives and well-being, free of preventable disease, disability, injury, and premature death. o Achieve health equity, eliminate disparities, and attain health literacy to improve health and well-being of all. o Create social and physical and economical environments that promote full potential for health and well-being for all. o Promote quality of life, healthy development and healthy behaviors and well-being across all life stages. o Engage leadership, key constituents, and public across multiple sectors to take action and design policies that improves the health and well-being of all. ▪ Physical Activity Objectives: o PA – 1: Leisure time physical activity o PA – 2: Adult aerobic physical activity and muscle strengthening activity o PA – 3: Adolescent aerobic physical activity and muscle strengthening activity o PA – 4: Daily physical education in schools o PA – 5: Adolescent participation in daily school physical education o PA – 6: Regularly scheduled recess o PA – 7: Time for recess o PA – 8: Child and adolescent screen time o PA – 9: Physical activity policies in child care settings o PA – 10: Access to school physical activity facilities o PA – 11: Physician counseling about physical activity o PA – 12: Worksite physical activity o PA – 13: Active transportation - walking o PA – 14: Active transportation - bicycling o PA – 15: Built environment policies
- 3. P a g e | 3 Dr. Nithin Ravindran Nair (PT) GENERAL HEALTH PROMOTION GOALS AND OUTCOMES 1) Impact of pathology / pathophysiology is reduced • Fitness level are improved • Health status is improved • Self-management of chronic disease is improved • Risk factors for development of injury reduced 2) Impact of impairments is reduced • Aerobic capacity – increased • Muscle endurance – increased • Gait, locomotion, and balance – improved • Motor function – improved • Muscle performance – increased • Postural control – improved • Relaxation - increased 3) Activity limitations are reduced • Ability to execute activities – improved • Tolerance of positions and activities – increased • Safety – improved • Problem solving and decision-making skills - enhanced 4) Participation restrictions are reduced • Ability to assume / resume required involvement in life situations - improved 5) Health, wellness and fitness are improved • Self-perceived health and wellness – improved • Understanding of health and wellness and health behaviors – increased • Self-efficacy – increased • Behaviors that support health and wellness – adopted • Self-management skills – improved • Intrinsic motivation – developed / increased 6) Societal resources are utilized • Awareness and use of community resources to support health and wellness - improved 7) Patient / Client satisfaction is enhanced • Therapeutic relationship with physiotherapist – valued by patient / client • Health coaching skills of physiotherapist – valued by patient / client
- 4. P a g e | 4 Dr. Nithin Ravindran Nair (PT) ROLE OF PHYSIOTHERAPISTS IN HEALTH PROMOTION: ▪ Physiotherapists can make a meaningful contribution to health of the nation by providing health and wellness to the population within their own practices. ▪ The role of physiotherapists in prevention, wellness and health promotion includes – ✓ Identifying risk factors and interventions to reduce risk in individuals and communities. For e.g., CAD Risk Factors Osteoporosis Risk Factors Dementia Risk Factors ▪ Family history ▪ Cigarette smoking ▪ Hypertension ▪ Hyperlipidemia ▪ Impaired fasting glucose level ▪ Obesity ▪ Sedentary lifestyle ▪ Bone mineral density score of – 2.5 or less ▪ Post-menopausal ▪ Caucasian or Asian descent ▪ Family history ▪ Low body weight ▪ Sedentary lifestyle ▪ Insufficient calcium and vit E ▪ Insufficient fruits and vegetables in diet ▪ Smoking ▪ Excessive consumption of Alcohol ▪ Prolonged bed rest ▪ Prolonged use of corticosteroids ▪ Less Education ▪ Hearing Loss ▪ TBI ▪ HTN ▪ Alcohol >21 units/week ▪ Obesity ▪ Smoking ▪ Depression ▪ Social Isolation ▪ Physical inactivity ▪ Air pollution ▪ Diabetes ✓ Preventing and slowing of progression of functional decline and disability and enhancing activities in those with a diagnosed condition. ✓ Reducing disability by restoring skills and independence in those with chronic conditions. ✓ Screening: Identifying individuals or groups who would benefit from education, intervention, or referral to an appropriate health care provider. ✓ Intervention: Providing intervention/prevention activities as identified from screening sessions. ✓ Consultation: Providing expertise and knowledge ✓ Education: Providing information on prevention, health, wellness, and fitness topics.
- 5. P a g e | 5 Dr. Nithin Ravindran Nair (PT) ✓ Critical Inquiry: Obtaining, synthesizing, and utilizing current research; interpreting data; and /or participating in research. ✓ Administration: Planning, developing, and managing all aspects of a prevention or wellness project including budget, human resources, and space. STEPS TO DEVELOP AND IMPLEMENT PREVENTION, HEALTH, WELLNESS AND FITNESS PROGRAM: STEP 1: IDENTIFY THE NEED ▪ Identify the intended audience – Children, adults, older adults, industry / business, school system, community, specific population. STEP 2: SET GOALS AND OBJECTIVES ▪ Identify the purpose of the program ▪ Identify the goals to be achieved – screening, education, intervention ▪ Identify objectives of the programs Example: Role of Physiotherapists in Health Promotion, Fitness and Wellness HEALTH PROMOTION, WELLNESS AND FITNESS Osteoporosis Screening: Perform osteoporosis assessment at community health fair. Critical Inquiry: Complete a literature review and identify most appropriate measures for osteoporosis. Education: Develop Community Education programs related to osteoporosis (importance of exercise, reducing falls in the home). Administration: Develop a resistance and weight -bearing exercise class. Falls Screening: Perform falls assessment at community health fair Critical Inquiry: Complete a literature review and identify most appropriate measures of fall risk Education: Develop Community Education programs related to fall prevention strategies. Intervention: Develop exercise program to increase strength, balance, flexibility, endurance in older adults. Work site Screening: Perform a work site assessment Consultation: Work with HRD of a company to identify ways to reduce work place injuries. Education: Educate employees and management on proper body mechanics, work station redesign, and ways to reduce injury risk. Intervention: Develop conditioning, work conditioning or work hardening program.
- 6. P a g e | 6 Dr. Nithin Ravindran Nair (PT) STEP 3: DEVELOP THE INTERVENTION ▪ Screening: Identify valid and reliable right tools to use for screening ▪ Education: Develop the program including handouts for participants ▪ Exercise: Develop plan for each class ▪ Logistics: ✓ Secure a location for the program ✓ Consider parking and access to the facility ✓ Determine the time and length of the program ✓ Determine the number of people who can attend based on the space ✓ Identify who will conduct the program (self / with assistance) ✓ Develop the presentation / program – include handouts for the participants ✓ Develop a budget, determine costs and charge to the participants STEP 4: IMPLEMENT THE INTERVENTION ▪ Be adaptable and be prepared for the unexpected. STEP 5: EVALUATE THE RESULTS ▪ For an educational session: Ask the participant to evaluate the program; consider an additional follow-up assessment ▪ For an exercise class: Record baseline data and assess progress during the program and at the end. ▪ Ask participants to evaluate the exercise program ▪ Ask for feedback on what could be done to improve the program HEALTH PROMOTION ACTION: (Ref: WHO CBR Guidelines) 5 areas for action which can be used to develop and implement health promotion strategies ✓ Build healthy public policy ✓ Create supportive physical and social environments for health ✓ Develop personal skills – provide information and health education ✓ Strengthen communities – adopt community approach, empower community ✓ Reorient health services towards health promotion
- 7. P a g e | 7 Dr. Nithin Ravindran Nair (PT) EXAMINATION AND EVALUATION (HEALTH PROMOTION AND WELLNESS) 1) Patient / Client History • Demographic History • Social History • Educational Qualification • Employment and work information • Living arrangements • General Health Status • Perceived Health and Perceived Wellness • Family History • Medical and Surgical History • Medications • Clinical Test Results • Functional Status and Activity Level • Past and Current Health Behaviors – Physical Activity, Smoking, Diet, Sleep, Stress Management, Substance Abuse 2) Systems Review • Cardiovascular • Pulmonary • Musculoskeletal • Neuromuscular • Integumentary • Communication Ability / Cognition / Learning Style 3) Test and Measures (Alphabetical order) • Aerobic Capacity / Endurance • Anthropometric Characteristics • Assistive Technology • Balance • Circulation • Community, Social and Civic Life • Cranial and Peripheral Nerve Integrity • Environmental Factors (Barriers) • Fitness Assessment • Gait Assessment
- 8. P a g e | 8 Dr. Nithin Ravindran Nair (PT) • Integumentary Integrity • Joint integrity and mobility • Mental Functions • Muscle Performance • Pain Assessment • Posture Assessment • Range of Motion • Self-Care and Domestic Life • Sensory integrity • Work Life MEASURES FOR HEALTH, WELLNESS, QUALITY OF LIFE, AND HEALTH BEHAVIOR CLINICAL MEASURES FOR HEALTH ✓ BMI ✓ Aerobic Capacity ✓ Blood Pressure ✓ Health Risk Appraisal Tool SELF PERCEIVED HEALTH, WELLNESS AND QOL MEASURES ✓ CDC Healthy Days Measure ✓ WHOQOL – Bref ✓ Medical Outcomes Short Form Health Survey (SF-36) ✓ Nottingham Health Profile ✓ Sickness Impact Profile (SIP) ✓ Dartmouth Cooperative Functional Assessment Charts (Dartmouth CO-OP Charts) ✓ Duke Health Profile ✓ Perceived Wellness Survey (PWS) DISEASE SPECIFIC MEASURES OF SELF PERCEIVED HEALTH, WELLNESS AND QOL MEASURES ✓ Arthritis Impact Measurement Scale (AIMS) ✓ Child Health Questionnaire (CHQ) ✓ Cystic Fibrosis Questionnaire ✓ European Organization for Research and Treatment of Cancer Quality of Life Measure (EORTC) ASSESSING HEALTH BEHAVIORS ✓ International Physical Activity Questionnaire (I-PAQ) ✓ Global Physical Activity Questionnaire (G-PAQ) PTO
- 9. P a g e | 9 Dr. Nithin Ravindran Nair (PT) INTERVENTIONS (Major 5 interventions) 1) Physical Activity / Exercise • Infants, Toddlers and Preschoolers Infants: (less than 1 year) ✓ Parents should play with infants several times a day during waking hours ✓ Infants should be encouraged to participate in a variety of activities that promote the development of basic movement skills – reaching, grasping, holding, squeezing, crawling, sitting, standing. ✓ For infants (not yet mobile) – 30 minutes of tummy time spread throughout the day while awake Toddlers: (1 – 2 years) ✓ At least 180 minutes (3 hours) per day in a variety of multiple bouts of short burst physical activities in both indoor and outdoor settings spread throughout the day. ✓ It should include at least 30 minutes of structured (directed by an adult) and 60 or more minutes of unstructured (initiated by the toddler) activity. Preschoolers (3 – 5 years) ✓ At least 180 minutes (3 hours) per day in a variety of multiple bouts of short burst physical activities in both indoor and outdoor settings spread throughout the day. ✓ It should include at least 60 minutes of structured (directed by an adult) and 60 or more minutes of unstructured (initiated by the infant) activity. • Children and Adolescents (6 – 17 years) ✓ 60 minutes of moderate (brisk walking) to vigorous (jogging or running) physical activity daily (mostly aerobic activity) ✓ At least 3 days a week activity should be vigorous ✓ Muscle strengthening activities, at least 3 days (≥ 60 mins/day) a week (gymnastics or pushup) ✓ Bone strengthening activities, at least 3 days (≥ 60 mins/day) a week (jumping rope or running) ✓ Activities should be age appropriate and fun • Adults ✓ Aerobic: Minimum 150 minutes (30 -60 minutes/day for 5 days/week) of moderate intensity aerobic activity (brisk walking) per week OR 75 minutes (20 - 30 minutes/day for 3 days/week) of vigorous intensity aerobic activity (jogging or running) per week OR equivalent mix of moderate and vigorous intensity aerobic activity (20 -30 minutes/day for 3-5 days/week). Moderate intensity: 5 – 6 RPE, Vigorous intensity: 7 – 8 RPE (0 – 10 SCALE)
- 10. P a g e | 10 Dr. Nithin Ravindran Nair (PT) ✓ Resistance: Muscle strengthening activities involving all major muscle group – 2 or more days per week. Each session: 2 – 4 sets of 8 – 12 repetitions and 2 – 3 minutes rest period between sets. ✓ Flexibility – At least 2 – 3 days per week (Hold for 30 -60 secs and repeat at least 4 times) For additional health benefits (lowering risk of colon / breast cancer): ✓ 300 minutes of moderate-intensity activity per week ✓ 150 minutes vigorous intensity activity, or ✓ A combination of moderate and vigorous intensity activity (30 -60 minutes/day for 3-5 days per week. • Older Adults ✓ Aerobic: Minimum 150 minutes (30 -60 minutes/day for 5 days/week) of moderate intensity aerobic activity (brisk walking) per week OR 75 minutes (20 - 30 minutes/day for 3 days/week) of vigorous intensity aerobic activity (jogging or running) per week OR equivalent mix of moderate and vigorous intensity aerobic activity (bouts of at least 10 minutes/day for 3-5 days/week). Moderate intensity: 5 – 6 RPE, Vigorous intensity: 7 – 8 RPE (0 – 10 SCALE) ✓ Resistance: Muscle strengthening activities involving all major muscle group – 2 or more days per week. Each session: 1 – 3 sets of 8 – 12 repetitions and 2 – 3 minutes rest period between sets. Light intensity – 40 -50% 1RM, Moderate to vigorous intensity – 60 – 80% 1RM. ✓ Flexibility: At least 2 – 3 days per week (Hold for 30 -60 secs and repeat at least 4 times) ✓ Include neuromotor exercises (balance exercises) to reduce risk of falls. • Adults with Disabilities ✓ Engage in regular physical activity according to their abilities and should avoid inactivity ✓ For substantial health gain aim for at least 150 minutes each week of moderate intensity activity ✓ Do strength and balance exercises at least 2 days per week • Pregnancy and Post-Partum ✓ Aerobic: Minimum 150 minutes (30 minutes/day for 5 days/week) of moderate intensity aerobic activity per week OR 75 minutes (20 - 30 minutes/day for 3 days/week) of vigorous intensity aerobic activity per week. (vigorous activity – only for women who were highly active prior to pregnancy Moderate intensity: 12 – 13 RPE, Vigorous intensity: 14 – 17 RPE (6 – 20 SCALE) ✓ Resistance: Muscle strengthening activities involving all major muscle group – 2 or more nonconsecutive days per week. Each session: 1 – 3 sets of 8 – 12 repetitions and 2 – 3 minutes rest period between sets.
- 11. P a g e | 11 Dr. Nithin Ravindran Nair (PT) ✓ Flexibility: At least 2 – 3 days per week (Hold for 10 -30 secs) ✓ For post-partum women – start pelvic floor exercise as soon as you can and continue daily 2) Smoking Cessation Counseling: 5 A’s and 5 R’s 5 A’s 5 R’s Ask about tobacco use Determine the Relevance of quitting to client Advise to quit Discuss the Risks of client’s continued tobacco use Assess readiness to quit Explore Rewards of quitting Assist in quit attempt Examine possible Roadblocks to quitting Arrange follow up Continue Repetition of the discussion 3) Healthy Weight and Healthy Eating Counseling ▪ Patient education: Impact of excessive weight and unhealthy eating on current condition and future health, importance of eating healthy, explain them about possible risk factors or consequences of obesity which are as follows - ✓ All causes of death mortality ✓ HTN ✓ Dyslipidemia ✓ Type 2 Diabetes ✓ CAD ✓ Stroke ✓ Gall Bladder Disease ✓ Osteoarthritis ✓ Sleep Apnea and respiratory problems ✓ Cancer (Endometrial, Breast, Colon, Kidney) ✓ Low QOL ✓ Clinical depression, anxiety ✓ Body pain and difficulty with physical functioning
- 12. P a g e | 12 Dr. Nithin Ravindran Nair (PT) ▪ Physiotherapists can screen for unhealthy eating behaviors and make basic recommendations for improving nutrition ▪ If possible, refer patients to a qualified health professional as appropriate. 4) Healthy Sleep Counseling ▪ Physiotherapists can evaluate sleep behavior using a sleep inventory questionnaire ▪ Physiotherapists are encouraged to discuss – adverse effect of insufficient sleep, Health problems found to be associated with insufficient sleep like HTN, diabetes, depression, obesity and cancer, discuss healthy sleep behaviors and provide basic recommendations for healthy sleep habits. 5) Stress Management ▪ Education: Difference between positive and negative stress, Find the triggers or stressors in life ▪ Relaxation Techniques – Deep Breathing, PMR, Mental Imagery, Meditation, Biofeedback, Mindfulness therapy ▪ Physical activity prescription to manage stress including yoga and tai chi ▪ Time management techniques ▪ Physiotherapists should recognize the need to refer the client to appropriate health professionals. THEORIES OF BEHAVIOR CHANGE ▪ It is essential for a physiotherapist to understand key theories of health behavior change to help client change their behavior: ▪ Major 4 theories are as follows: ✓ Health Belief Model ✓ Theory of Reasoned Action and Theory of Planned Behavior ✓ Transtheoretical Model ✓ Social Cognitive Theory
- 13. P a g e | 13 Dr. Nithin Ravindran Nair (PT) Health Belief Model Theory of Reasoned Action and Theory of Planned Behavior Transtheoretical Model (TTM) STAGES OF CHANGE PROCESSES OF CHANGE DECISIONAL BALANCE SELF EFFICACY Perceived susceptibility to disease Perceived seriousness to disease Cues to action Demographic and sociopsychological variables Perceived threat of disease Self-efficacy Likelihood of taking recommended action Perceived benefits and barriers of taking recommended action Attitude toward behavior Behavior Behavioral intention Perceived behavioral control Subjective Norm Constructs in the TTM
- 14. P a g e | 14 Dr. Nithin Ravindran Nair (PT) STAGE OF CHANGE PRECONTEMPLATION CONTEMPLATION PREPARATION ACTION MAINTENANCE TERMINATION DOES NOT INTENTED TO TAKE ACTION WITHIN 6 MONTHS INTENDS TO TAKE ACTION WITHIN 6 MONTHS INTENDS TO TAKE ACTION WITHIN THE NEXT 30 DAYS + TAKEN PRELIMINARY STEPS ENGAGED IN THE BEHAVIOR FOR LESS THAN 6 MONTHS ENGAGED IN THE BEHAVIOR FOR MORE THAN 6 MONTHS ENGAGES IN BEHAVIOR + HIGH SELF EFFICACY + NO TEMPTATION TO RETURN TO UNHEALTH BEHAVIOR
- 15. P a g e | 15 Dr. Nithin Ravindran Nair (PT) PROCESS OF CHANGE: COGNITIVE PROCESSES STAGE BEHAVIORAL PROCESSES STAGE Conscious Raising (Increasing Knowledge) PC - C Self-Liberation (Committing to Change) P Dramatic Relief (Awareness of Risks of Physical Inactivity) PC - C Counter Conditioning (Substituting Healthy Alternatives) A - M Environmental Re-evaluation (Caring About Consequences to Others) PC - C Helping Relationships (Seeks Social Support) A - M Self-Re-evaluation (Self-Image & Personal Values) C Reinforcement Mx (Using Rewards) A - M Social Liberation (Society Is Supportive for Change) P Stimulus Control (Reminders and Cues for Healthy Behaviour) A - M PC – PRECONTEMPLATION, C - CONTEMPLATION, P – PREPARATION, A – ACTION, M – MAINTENANCE
- 16. P a g e | 16 Dr. Nithin Ravindran Nair (PT) DECISIONAL BALANCE ▪ Process of weighing the pros and cons of changing the behaviour ▪ For example: In the beginning (more cons) as the client gains experience (more pros) STAGES OF CHANGE DECISIONAL BALANCE PC - C Pros < Cons C - P Pros > Cons P - A Pros >> Cons A - M Pros >> Cons SELF EFFICACY ▪ Good predictor of physical activity ▪ Strategies for promoting self-efficacy ✓ Past successes with physical activity ✓ Praise the client ✓ Express confidence (ability to reach goal) ✓ Encourage the client to observe similar others STAGES OF CHANGE SELF-EFFICACY PC - C Low C - P Increases P - A High A - M High PC – PRECONTEMPLATION, C - CONTEMPLATION, P – PREPARATION, A – ACTION, M – MAINTENANCE PC – PRECONTEMPLATION, C - CONTEMPLATION, P – PREPARATION, A – ACTION, M – MAINTENANCE
- 17. P a g e | 17 Dr. Nithin Ravindran Nair (PT) SOCIAL COGNITIVE THEORY: It is a model of interpersonal health behavior OTHER MODELS: PHYSICAL ACTIVITY MODEL FOR PWD: ▪ Developed to explain the behavior of PA in a population of PWD. ▪ It integrates behavioral theoretical models with disability models and uses the ICF framework and terminology. COMMUNITY MODELS ▪ Precede-Proceed planning model. ENVIRONMENT PERSONAL FACTORSBEHAVIOR
- 18. P a g e | 18 Dr. Nithin Ravindran Nair (PT) HEALTH PROMOTION MODELS ▪ Health protection / disease prevention is one of the most accepted models. ▪ Interventions in this model are categorized as – primordial, primary, secondary and tertiary prevention Pre – Pathogenesis Pathogenesis Prevention of occurrence of disease Prevention of progression of disease 1. Primordial Prevention 2. Primary Prevention ✓ Health Promotion ✓ Specific Protection 1. Secondary Prevention ✓ Early Diagnosis and Prompt Treatment 2. Tertiary Prevention ✓ Disability Limitation ✓ Rehabilitation REFERENCES: ❖ Principles and Practice of Physical Rehabilitation – Neeta J Vyas et. al. ❖ Therapeutic Exercise: Foundations and Techniques – Carolyn Kisner et. al. ❖ Physical Rehabilitation – Susan B. O’Sullivan et. al. ❖ ACSM’s Guidelines to Exercise Testing and Prescription – 10th ed ❖ ACSM’s Complete Guide to Health and Fitness – Barbara Bushman ❖ UK Chief Medical Officers’ Physical Activity Guidelines, 2019