ACTEP2014: Sepsis marker in clinical use
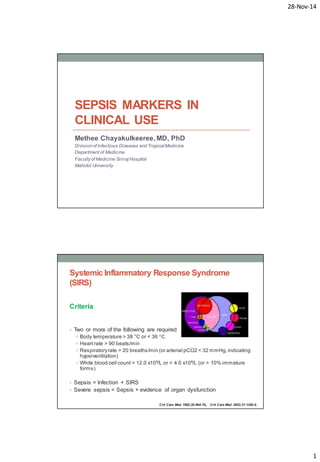
- 1. 28-Nov-14 1 SEPSIS MARKERS IN CLINICAL USE Methee Chayakulkeeree, MD, PhD Division of Infectious Diseases and Tropical Medicine Department of Medicine Faculty of Medicine Siriraj Hospital Mahidol University Systemic Inflammatory Response Syndrome (SIRS) Criteria • Two or more of the following are required Body temperature > 38 °C or < 36 °C Heart rate > 90 beats/min Respiratory rate > 20 breaths/min (or arterial pCO2 < 32 mmHg, indicating hyperventilation) White blood cell count > 12.0 x109/L or < 4.0 x109/L (or > 10% immature forms) • Sepsis = Infection + SIRS • Severe sepsis = Sepsis + evidence of organ dysfunction Crit Care Med 1992;20:864-74., Crit Care Med 2003;31:1250-6.
- 2. 28-Nov-14 2 Diagnostic Criteria for Sepsis Infection, documented or suspected, and some of the following: General variables • Fever (> 38.3°C) • Hypothermia (core temperature < 36°C) • HR > 90/min or > 2 SD above normal value for age • Tachypnea • Altered mental status • Significant edema or positive fluid balance (> 20 mL/kg over 24 hr) • Hyperglycemia (plasma glucose > 140 mg/dL or 7.7 mmol/L) in the absence of diabetes Inflammatory variables • Leukocytosis (WBC count > 12,000 /μL) • Leukopenia (WBC count < 4000 /μL) • Normal WBC count with > 10% immature forms • Plasma C-reactive protein > 2 SD above normal value • Plasma procalcitonin > 2 SD above the normal value Hemodynamic variables • Arterial hypotension (SBP < 90 mm Hg, MAP < 70 mm Hg, or an SBP decrease > 40 mm Hg in adults or < 2 SD below normal for age) Organ dysfunction variables • Arterial hypoxemia (Pao2/Fio2 < 300) • Acute oliguria (urine output < 0.5 mL/kg/hr for at least 2 hrs despite adequate fluid resuscitation) • Creatinine increase > 0.5 mg/dL or 44.2 μmol/L • Coagulation abnormalities (INR > 1.5 or aPTT > 60 s) • Ileus (absent bowel sounds) • Thrombocytopenia (platelet count < 100,000 /μL) • Hyperbilirubinemia (plasma total bilirubin > 4 mg/dL or 70 μmol/L) Tissue perfusion variables • Hyperlactatemia (> 1 mmol/L) • Decreased capillary refill or mottling Surviving Sepsis Campaign Guidelines. Crit Care Med. 2013;41:580-637. Severe sepsis = sepsis-induced tissue hypoperfusion or organ dysfunction • Sepsis-induced hypotension • Lactate above upper limits laboratory normal • Urine output < 0.5 mL/kg/hr for > 2 hrs despite adequate fluid resuscitation • Acute lung injury with Pao2/Fio2 < 250 in the absence of pneumonia as infection source • Acute lung injury with Pao2/Fio2 < 200 in the presence of pneumonia as infection source • Creatinine > 2.0 mg/dL (176.8 μmol/L) • Bilirubin > 2 mg/dL (34.2 μmol/L) • Platelet count < 100,000 μL • Coagulopathy (international normalized ratio > 1.5) Surviving Sepsis Campaign Guidelines. Crit Care Med. 2013;41:580-637.
- 3. 28-Nov-14 3 Two phases of sepsis: Sequential Model Pro-inflammatory cytokines: TNF, IL-1β, IL-6, CRP, PCT Anti-inflammatory cytokines: IL-10 Hyper-inflammatory phase: SIRS Immunosuppressed phase: Compensatory anti-inflammatory response syndrome (CARS) Contrib Microbiol 2011;17:1–11., Chest 1997;112:235–43. Two phases of sepsis: Concurrent Model Infect Dis Clin North Am 1999;13:413–26.
- 4. 28-Nov-14 4 Sepsis Biomarkers • Acute phase proteins CRP Procalcitonin (PCT) Pentraxin3 (PTX3) Lipopolysaccharide binding protein (LBP) • Cytokines & chemokines IL-1RA, IL-1b, IL-2, IL-6, MCP-1 TNF-a, TNFR1/2 HMGBP1 • Cell surface markers Soluble CD14 (presepsin) Neutrophil CD64 index (CD64in) mHLA-DR (monocyte HLA-DR levels) CD-163 • Receptor markers VEGF Soluble VEGF-receptor 1 (sFLT) Soluble urokinase plasminogen activator (suPAR) sTREM-1 RAGE (soluble receptor for advanced glycationend products) • Coagulation Activated partial thromboplastin time (aPTT) waveform analysis Protein C receptor Thrombomodulin • Endothelial damage Heparin binding protein E-selectin Neopterin ICAM-1, VCAM-1 Angiopoietin-1 and -2 Syndecan-1 and -2 • Vasodilation Copeptin (AVP precursor) • Cell damage MicroRNA Microparticles • Cell repair Procollagen III amino propeptide inflammation coagulation Tissue damage and repair Pro-inflammatory cytokines during hyper-inflammatory phase of sepsis PAMPs = Pathogen Associated Molecular Patterns DAMPs = Damage Associated Molecular Patterns Crit Rev Clin Lab Sci, 2013; 50: 23–36
- 5. 28-Nov-14 5 Interleukin-6 (IL-6) • A pro-inflammatory cytokine • More reliably measurable in plasma than TNF and IL-1β • Not specific for sepsis (like TNF and IL-1β) • Autoimmune rheumatic disorders • Major role as a biomarker of sepsis appears to be prognostic, not diagnostic • Elevated levels of IL-6 in septic patients are associated with an increase in mortality Br J Surg 1994;81:1306–8., Intensive Care Med 2002;28:1220–5., Crit Care Med 2004;32:2173–82. C- reactive protein (CRP) • One of a group of acute phase reactants • A well-established biomarker of infection and inflammation • Inflammatory or infectious disease • Atherosclerosis • Cardiovascular disease • High sensitivity, low specificity • Also use for monitoring in pediatric and post-operative patients N Eng J Med 1999;340:448–54.
- 6. 28-Nov-14 6 Procalcitonin (PCT) • A peptide precursor of the hormone calcitonin • Composed of 116 amino acids with a half-life of 25 to 30 hours • Produced by parafollicular cells (C cells) of the thyroid and the neuroendocrine cells of the lung and the intestine • Level in healthy individuals is below the limit of detection (10 pg/mL) • Rises in a response to a pro-inflammatory stimulus, especially of bacterial origin (not in viral infection or non-infectious inflammations) • Produced mainly by the cells of the lung and the intestine • High procalcitonin levels produced during infections are not followed by a parallel increase in calcitonin or a decrease in serum calcium levels. Lancet Infect Dis 2013;13: 426–35
- 7. 28-Nov-14 7 Procalcitonin-guided interventions against infections in ICU: an RCT Procalcitonin-guided interventions against infections in ICU: an RCT Crit Care Med 2011; 39:2048 –2058
- 8. 28-Nov-14 8 Conclusion from the study • A strategy with escalation of broad spectrum antimicrobials in the intensive care unit guided by daily procalcitonin measurements as used in this trial did NOT improve survival and did lead to an increased use of broad-spectrum antimicrobials, which is concerning in regard to toxicity, resistance, and economics. • We observed deleterious effects on organ function and length of stay in the intensive care unit and the strategy cannot be recommended. Crit Care Med 2011; 39:2048 –2058 Biomarkers of activated neutrophils and monocytes in sepsis Neutrophil Macrophage
- 9. 28-Nov-14 9 Four Promising Biomarkers for Acute Infection •sTREM-1 •suPAR •ProADM •sCD14 (Presepsin) LBP and sCD14 (Presepsin) • Elevated levels of LBP can identify patients with infection, but this protein effectively neutralizes LPS, and may even be anti-inflammatory • Therefore, LBP may be less discriminating than other biomarkers with regard to risk of developing severe sepsis • Recently, there has been interest in measuring a soluble form of CD14 (Presepsin) as a biomarker of sepsis. • Soluble CD14 levels were shown to be comparable to PCT for diagnosis of bacterial infection and correlated with the degree of severity in septic patients J Infect Chemother 2012;18:891–7., J Infect Chemother 2011;17:764–9.
- 10. 28-Nov-14 10 Soluble CD14-subtype (sCD14-ST) • CD14 is a 13 kDa protein that is present in macrophage, monocyte, and granulocyte cells and their cell membranes • Responsible for intracellular transduction of endotoxin signals • Its soluble fraction is present in blood and is thought to be produced in association with infections J Infect Chemother 2011;17:764–9. sCD14 in Clinical Use Annals of Intensive Care 2013, 3:22.
- 11. 28-Nov-14 11 sCD14 Value in Different Conditions J Infect Chemother 2011;17:764–9. sCD14 and Other Biomarkers in Sepsis Infection vs. non-infection SIRS: infection vs. sepsis J Infect Chemother 2011;17:764–9.
- 12. 28-Nov-14 12 sCD14 and APACHE II Score J Infect Chemother 2011;17:764–9. sCD14 in Emergency Department Critical Care 2013, 17: R244
- 13. 28-Nov-14 13 sCD14 in Emergency Department Diagnosis of sepsis Predicting severe sepsis Critical Care 2013, 17: R244 Multicenter, Randomized ALBIOS Trial - sCD14 and Organ Failure Total 997 patients 1 = <597 ng/L 2 = 597-1397 ng/L 3 = >1397 ng/L Intensive Care Med. 2014 Oct 16
- 14. 28-Nov-14 14 ALBIOS Trial: Appropriateness of ATB Therapy and sCD14 Intensive Care Med. 2014 Oct 16 ALBIO Trial: Day 1 sCD14 Concentration and Mortality Intensive Care Med. 2014 Oct 16
- 15. 28-Nov-14 15 ALBIOS Trial: Changes in sCD14 and Mortality Intensive Care Med. 2014 Oct 16 D1-2 1st : < -14.9 2nd : -14.9-13.7 3rd : > 13.7 D1-7 1st : < -38.4 2nd : -38.4- 15.8 3rd : > 15.8 Burn Sepsis Burns. 2014;40:664-9
- 16. 28-Nov-14 16 Burn Sepsis Burns. 2014;40:664-9 Abdominal Sepsis Intra-abdominal infections Sample size: Healthy 70, SIRS 30, Sepsis 20, Severe sepsis 10 Clin Chem Lab Med 2013;51:2053-62
- 17. 28-Nov-14 17 sCD14 in Sepsis vs SIRS (non-infection) Area under ROC sCD14: 0.996 PCT: 0.912 CRP: 0.857 WBC: 0.777 Clin Chem Lab Med 2013;51:2053-62 Biomarkers in Febrile Neutropenia in Pediatric Oncology Patients Cytokine 2013:62:34-37
- 18. 28-Nov-14 18 sCD14-ST in Adult Febrile Neutropenia • Preliminary data from Siriraj Hospital • Total = 25 • Male 12 (48%), female 13 (52%) • Mean age 43 ± 11 years • Underlying diseases • AML 14 (56%) • ALL 4 (16%) • CML 1 (4%) • NHL 5 (20%) • Other 1 (4%) Bacteremia and Biomarkers sCD14-ST Procalcitonin * * *
- 19. 28-Nov-14 19 Summary • Biomarkers are promising for use for diagnosis and prognosis in sepsis as well as initiation and determination of antimicrobial therapy • Biomarkers available for clinical use include PCT, CRP, IL6 and sCD14 • Increasing data of sCD14-ST for clinical use in intensive care and emergency department THANK YOU FOR YOUR ATTENTION
